|
Diffuse peritoneal
deciduosis in pregnancy: A case report
......................................................................................................................................................................
Nansi Al Fayez
Basel Khreisat
Department of Obstetrics and Gynecology,
King Hussein Medical Center,
RMS, Jordan
Correspondence:
Nansi AlFayez MD
Department of Obstetrics and Gynecology,
King Hussein Medical Center,
RMS, Jordan
Email: nancy_ghishan@yahoo.com
Deciduosis or ectopic decidua
is the presence of a group of decidual cells outside
the endometrium. Walker was the first to define
the condition in 1887(1). In pregnancy, the occurrence
of ectopic deciduas was observed in ovaries, uterus
and tubes, while localization in peritoneum was
rare(2-6). It is important to differentiate between
this benign phenomena and Mesothelioma , malignant
carcinoma and metastatic malignant Melanoma(7,8).
We are reporting a case of ectopic deciduas in
a 27-year -old lady who was asymptomatic during
the course of her pregnancy, presented with preterm
labour pain, and underwent ceasarean section due
to Triplet pregnancy. The lesions were discovered
accidentally; they were nodular covering most
of the peritoneum and there was omental cake.
Biopsies were taken to differentiate it from malignant
conditions. Histopathological diagnosis confirmed
deciduosis.
A 30-year-old lady, P0+1, 28
weeks pregnant with triplets, her pregnancy is
a product of intrauterine insemination after a
few years of secondary infertility. Her pregnancy
was smooth till a few hours prior to presentation
when she started to complain of labor like abdominal
pain; on examination she was found to have 4 cm
dilated cervix shortening in its length. She underwent
emergency caesarean section, and after closure
of the uterus, inspection of abdominal cavity
revealed presence of whitish nodules on the tubes,
ovaries, meso- colon(picture 1) and extensive
nodularity of the omentum forming omental cake.
Biopsies were taken from the nodules, and the
omentum; they were sent for histopathology. Peritoneal
wash was sent for cytology. The immunohistopathology
confirmed the diagnosis of ectopic decidua. Eight
weeks later the patient underwent diagnostic laparoscopy
as follow up; the lesions were resolved completely
(pictures 2,3,4).
Figure 1: Diffuse nodularity of meso-colon
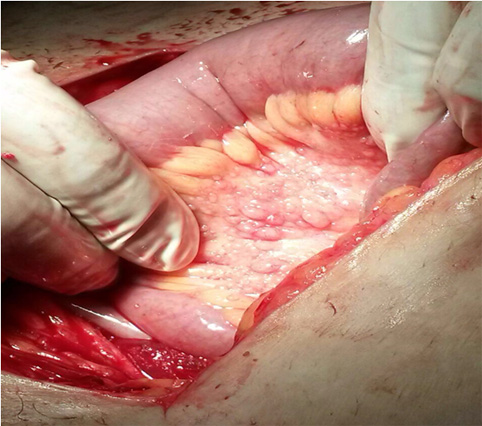
Figure 2: pelvic side wall 8 weeks post cesarean
section

Figure 3: pelvic side wall
with ovary and tube 8 weeks post cesarean section
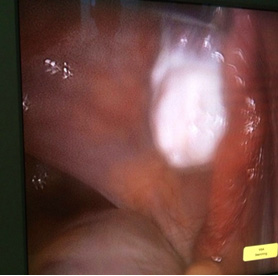
Figure 4: pouch of Douglas
8 weeks post cesarean section

Extensive peritoneal deciduosis
is a rare condition(2-6,9). It is seen in ovaries,
uterine serosa, pelvic side wall, bowel and omentum.
The macroscopic intraoperative appearance suggests
peritoneal carcinomatosis, as we have in our case.(10)
Ectopic deciduas could be seen in the appendix,
diaphragm, spleen, liver renal pelvis and paraaortic-pelvic
lymph nodes(9,11-14). It has been documented to
occur mostly in other sites of Mullerian origin(15-17).
The majority of ectopic
deciduas cases has been associated with progesterone
secreting corpus luteum in pregnancy(6-8). A diffuse
form is uncommon and occurs in the conditions
of high levels of progesterone, most commonly
seen in pregnant women with multigestation(15-17)
as we have in our case. In the absence of pregnancy,
the stimulation of ectopic decidual cells attributed
to progesterone secreted from adrenal cortex.(7)
Deciduosis is usually
asymptomatic during pregnancy, and discovered
accidentally during ceasarean section(18). Cases
of pseudo-acute appendicitis, haemoperitoneum,
cutaneous swellings and abnormal appearance of
cervix have been reported in pregnancy(19,20).
Malpica et al, reported a case of obstructed labour
due to gross peritoneal deciduosis in 2002.(21)
The appearance of peritoneal deciduosis ranges
from geographic pattern, nodular distribution
to polypoid appearance(7-9,16 ). In our case they
were in the form of multiple small nodules.
Diffuse lesions on the omentum are seen on the
peritoneal surface as grey-white multiple and
presence of focal haemorrhagic nodules or plaques,
detected intraoperatively, as we saw in our case.
They should be differentiated from peritoneal
tuberculosis or metastatic lesions and can be
confused in frozen section(6-9,13).
On histopathological examination, it is important
to differentiate ectopic deciduas from deciduoid
malignant mesothelioma, metastatic malignant melanoma
and vacuolated decidual cells from metastatic
signet ring cell carcinoma.
Deciduoid Mesothelioma is a variant of Mesothelioma
that can be seen in a wide range of ages, with
similar outcome as epithelioid mesothelioma(23,24);the
cells are large, with well defined borders, abundant
eosinophilic cytoplasm, little pleomorphism, low
mitotic activity and cohesive.(23)
Signet ring cell carcinomatosis have cells with
eccentric nuclei, mucin filled cytoplasm and diffuse
infiltrating cells that can be found in the form
of single cells, cords and nests.(25)
The diagnosis of deciduoid mesothelioma will be
supported by positivity of cytokeratin 5/6 and
calretinin on immunohistochemical analysis, while
the HMB-45 S-100 protein and keratin positivity
metastatic carcinoma support malignant melanoma.(26,27)
The clinical history, the lack of mitosis in decidual
cells, negativity of calretinin, keratin, HMBE-1
and vimentin and PR positivity on immunohistochemical
analysis support deciduosis.(8,26,27)
Deciduosis or ectopic deciduas
represents a physiological reaction of pleuripotent
stromal cells to stimulation of progesterone.
It is a benign lesion, and resolves spontaneously
in the postpartum period. Nodules should be biopsied
during surgery to be differentiated from malignancy.
1. Walker A: Der Bau der Eihaeute
bei Graviditatis abdominalis. Virchows Arch Path
Anat 1887, 197:72-99
2. Israel SL et al.: The ovary at term. I. Decidua-like
reaction and surface cell proliferation. Obstetrics
Gynecology 1954, 3:399-407
3. Ober WB, Grady HG, Schoenbucher AK: Ectopic ovarian
decidua without pregnancy. American Journal of Pathology
1957, 23:199-217.
4. Schneider V, Barnes LA: Ectopic decidual reaction
of the uterine cervix: frequency and cytologic presentation.
Acta Cytol 1981, 25:616-622
5. Hofbauer J: Decidual formation on the peritoneal
surface of the gravid uterus. American J Obstet
Gynecol 1929, 17:603-612
6. Shukla S et al.: Ectopic decidual reaction mimicking
peritoneal tubercles: a report of three cases. Indian
J Pathology Microbiology 2008, 51:519-520
7. Büttner A et al.: Pregnancy-associated ectopic
decidua (deciduosis) of the greater omentum. An
analysis of 60 biopsies with cases of fibrosing
deciduosis and leiomyomatosis peritonealis disseminata.
Pathology Res Pract 1993, 189:352-359
8. Kondi-Pafiti A et al.: Ectopic decidua mimicking
metastatic lesions-report of three cases and review
of the literature. European J Gynaecol Oncol 2005,
26:459-461.
9. Clement PB: Diseases of the Peritoneum. In Kurman
RJ. (Ed): Blaustein's Pathology of the Female Genital
Tract. 5th ed., New York, Springer, 2002, 729-789
10. Malpica A et al. Gross deciduosis peritonei
obstructing labour : a case report and review of
the literature. International J Gynecol Pathol.
2002;21:273-275
11. Lesaffer J et al.: Pregnancy-associated ectopic
decidua of the appendix. Acta Chir Belg 2009, 109:93-94.
12. Suster S, Moran CA: Deciduosis of the appendix.
American J Gastroenterol 1990, 85:841-845
13. Wu DC et al: Ectopic decidua of pelvic lymph
nodes: a potential diagnostic pitfall. Arch Pathol
Lab Med 2005, 129:e117-120.
14. Bettinger HF: Ectopic decidua in the renal pelvis.
J Pathol Bacteriol 1947, 59:686
15. Machida S et al. Decidualization of ovarian
endometriosis during pregnancy mimicking malignancy:
report of three cases with a literature review.
Gynecology Obstetrics Invest 2008; 66: 241-247
16. Zaytsev P et al. Pregnancy-associated ectopic
decidua. American J Surg Pathol 1987; 11: 526-530
17. Ellis CL et al. Ectopic decidua in abdominal
washings found intraoperatively at cesarean section.
Diagnostic Cytopathology 2010; 38: 740-741
18. Tang LC et al. Intraperitoneal bleeding from
ectopic decidua following hormonal contraception.
Case report. British J Obstet Gynaecol. 1985 Jan;
92(1):102-3.
19. Richter MA et al. Bleeding ectopic deciduas
as a cause of intraabdominal haemorrhage. A case
report. Journal of Reproductive Medicine 1983 Jun;
28(6):430-2.
20. Flieder DB et al. Pleuro-pulmonary endometriosis
and pulmonary ectopic deciduosis: a clinicopathological
and immunohistochemical study of 10 cases with emphasis
and diagnostic pitfalls. Human Pathology.1998 Dec;29(12):1495-503.
21. Malpica A et al. Gross deciduosis peritonei
obstructing labor: a case report and review of literature.
International J Gynaecol Pathol. 2002 Jul;21(3):273-5.
22. Massi D et al. : Pregnancy-associated ectopic
deciduas . Acta Obstet Gynecol Scand 1995, 74:568-571.
23. Shanks JH et al. Mesotheliomas with deciduoid
morphology: a morphologic spectrum and a variant
not confined to young females. American J Surg Pathol
2000; 24: 285-294.
24. Ordonez NG. Deciduoid mesothelioma: report of
21 cases with review of the literature. Mod Pathol
2012; 25: 1481-1495.
25. Lee EY et al. Late recurrence of malignant melanoma
presenting as peritoneal "carcinomatosis".
Abdom Imaging 2003; 28: 284-286
26. Mourra N et al.: Malignant deciduoid mesothelioma:
a diagnostic challenge. Arch Pathol Lab Med 2005,
129:403-406.
27. Reis-Filho JS et al. : Primary epithelial malignant
mesothelioma of the pericardium with deciduoid features:
cytohistologic and immunohistochemical study. Diagnostic
Cytopathology 2002, 26:117-122
|