|
Effectiveness
of an Interventional Program for the Management
of Hypertension through Strengthening of the Health
Care Delivery System: a Pilot Study
.............................................................................................................................................................................
Waris Qidwai (1)
Khawar Kazmi (2)
Kashmira Nanji (3)
Sana Anees (4)
(1) Dr. Waris Qidwai
Professor and Chairman
Department of Family Medicine
The Aga Khan University, Karachi
(2) Dr. Khawar Kazmi
Professor of Cardiology
Department of Medicine
Aga Khan University, Karachi
(3) Kashmira Nanji
Senior Instructor (Research)
Department of Family Medicine,
Aga Khan University, Karachi
(4) Sana Anees
Research Associate
Department of Family Medicine,
Aga Khan University, Karachi
Correspondence:
Dr. Waris Qidwai
The Tajuddin Chatoor
Professor and Chairman
Department of Family Medicine
Aga Khan University, Karachi
Stadium Road, PO Box: 3500
Karachi-74800, Pakistan
Tel: 92-21-3486-4842 (Office) 92-3332317836 (Cell)
Email: waris.qidwai@aku.edu
|
ABSTRACT
Background: The aim of the study was
to assess the effectiveness of an interventional
program to improve hypertension management
through strengthening of the health care
delivery system.
Methods: A pilot study was conducted
from February to December 2014 in two off-site
Family Medicine clinics of the Aga Khan
Hospital Karachi, Pakistan. Patients aged
> 40 years, with known hypertension
were included. At the intervention site,
Family Physicians were trained; individual
and group education sessions were conducted
for catchment population, while usual care
was provided at the control site. Referral
system between primary, secondary and tertiary
levels of care was strengthened. Data was
entered and analyzed in SPSS version 19.
T-test for independent sample was used for
comparison between intervention and control
groups.
Results: 118 patients were recruited
but 90 patients (44 intervention, 46 control
group) were included in the final analysis.
Mean age of patients in intervention group
was 50.5+ 8.7 years in comparison to 52.0
+8.3 years in the control group. A statistically
significant mean difference was observed
in systolic BP control in the intervention
group (140.2 + 14.6 mm Hg) after a follow-up
of six months. There was a significant difference
in the mean scores of satisfaction levels
between intervention (3.9 + 0.2) and control
groups (3.7 + 0.2, P=0.003). Post intervention,
55% of patients in the intervention group
and 39% in the control group were taking
antihypertensive medications regularly.
Conclusion: Intervention at primary
care level along with strengthening of the
health care delivery system should be undertaken
to better manage hypertension.
Key words: Hypertension, Primary Care,
Family Physician, Health Care System
|
Hypertension is an emerging public
health challenge globally; with an increasing
prevalence in developing countries.(1) Adverse
impact of huge disease burden, arising from hypertensive
patients in developing countries, is made worse
because of weak health care delivery and lack
of resources. Despite such adverse condition awareness,
treatment and control of blood pressure among
hypertensive patients is improving in these countries.(2,
3)
Pakistan is a developing country and 33% of the
adult population suffers from hypertension.(4)
This huge disease burden puts immense pressure
on limited resources. A recent study has reported
blood pressure control in accordance to guidelines,
among 30.8% of hypertensive patients in Pakistan.(5)
An earlier study has reported younger age and
poor awareness about hypertension as factors that
adversely affect adherence to antihypertensive
medication and blood pressure control among hypertensive
patients in Pakistan.(6)
Primary care is the frontline of a health care
delivery system where patients are screened and
managed for hypertension. It has been shown that
strengthening of primary care can result in better
blood pressure control among hypertensive patients.(7)
It has been reported that training of General
Practitioners in management of hypertensive patients
results in better blood pressure control among
patients in their clinical care.(8)
Limited evidence is available from Pakistan on
effectiveness of intervention aimed at strengthening
the primary care and health care system to effectively
control hypertension. Based on this identified
need, we conducted a trial on effectiveness of
strengthening the primary care and health care
delivery system to effectively control hypertension.
Study Settings:
A quasi-experimental study was conducted in two
off-site "Integrated Medical Services"
Family Medicine clinics, Aga Khan University Hospital
Karachi, Pakistan, from February 2014 to December
2014. Integrated Medical Services (IMS) are community
based health care facilities that offer Family
Medicine services in addition to diagnostic support.
Patients:
Individuals aged 40 years or more, visiting the
selected IMS centers with known hypertension or
with consistently elevated BP on two separate
visits (mean of last two of three measurements
of systolic pressure > 140 mm Hg or
mean diastolic pressure > 90 mm Hg)
or already receiving treatment, were recruited
in the study.
Those patients who require intensive care unit
or coronary care unit admissions, or were diagnosed
to have cognitive impairment, were agitated due
to severe pain, non-resident of Karachi, or having
language barrier were excluded from the study.
Intervention:
Intervention arm:
Multiple interventions were used including training
of family physicians, patient health education
sessions and development of a referral system
with secondary and tertiary levels of health care.
Training of Family Physician: Consultant
Family Physicians conducted training sessions
for Family Physicians regarding hypertension and
they were given updated information for its management.
Patient Education Sessions: Patients
in the intervention arm were provided with individual
counseling during which the participants were
given detailed information regarding their disease
process, optimum blood pressure levels, lifestyle
modification (exercise and diet) and importance
of adherence to treatment. Participants were also
given written brochures/pamphlets about hypertension
management. The education session was conducted
by a Research Medical Officer (RMO) who was trained
for this task by a Consultant Physician. The Family
Physician also provided customized education to
patients according to their needs.
Initiating a Referral system (primary-secondary-tertiary)
for hypertension management:
Primary care: Patients with uncomplicated
hypertension were managed by the Family Physician
at the IMS clinics. Those with complicated hypertension
such as with target organ damage, CVD, CKD or
needing more than 3 drugs were referred for secondary
care.
Secondary care: Community Health Center,
Aga Khan University Hospital served as the secondary
care service provider. Patients with CVD, CKD
or needing more than 3 drugs, not responding to
treatment, or patients with secondary hypertension
were referred to tertiary care level.
Tertiary care: Cardiologist at AKU managed
secondary, resistant and difficult to treat hypertension.
The patients were then referred back to the Family
Physician at primary care level.
Control Arm: Standard Care: Patients coming
to the control clinic of IMS were given usual
hypertension care received
at the IMS centers.
Outcome Ascertainment:
The primary outcome was to observe a difference
of at least 20 points in the blood pressure levels
among the intervention and control groups within
06 months of follow-up. The other secondary outcomes
of this study were: adherence to life style modification
(exercise, and medication) by the patients. Cost
of hypertension treatment, this included: cost
of medication (self-report by patient), cost of
physician visit (clinic data), and cost of laboratory
work. Patient Satisfaction to the care was inquired
through PSQ-18. (9) It is a short form of the
PSQ III which has 80 questions and includes seven
dimensions of satisfaction that is general satisfaction,
technical quality, interpersonal manner, communication,
financial aspects, time spent with doctor, and
accessibility and convenience.
Baseline Assessment:
Baseline assessment included detailed history,
physical examination, laboratory investigations
and a care plan.
Follow up visits:
At 3 and 6 months: Patients in both arms
were reassessed at 03 and 06 months intervals
and outcome assessment was carried out. The study
covered anthropometric measurements, blood pressure
assessment and lab investigations. Adherence to
medications and life style modification (diet,
exercise) were evaluated through self-report and
counting of empty medication blisters.
Questionnaire Development: The questionnaire
was initially developed in English language and
was then translated into local language and back
translated in English. The consistency in the
back translated questionnaire was checked by the
principal investigator/co-investigators, and any
discrepancies found were removed.
Ethical Consideration: The study was reviewed
and approved by the Ethical Review Committee of
Aga Khan University. The trial was also registered
at clinical trial.gov (NCT02186067).
Written Informed Consent was obtained from all
participants after explaining to them about the
study protocol. All study personnel were trained
in procedures for maintaining patient confidentiality.
No personal identifiers were used in any report
or publication arising from this study.
Statistical Analysis:
Sample Size: The study was designed to
enroll 90 patients (45 patients in each group).
This number of patients would provide the study
with the ability to detect a 20 percent difference
among groups (treatment and control) in six months
with a power of 80%. The proportion in the treatment
group is assumed to be 0.60. The sample size was
calculated using NCSS PASS.
Analysis: Data was entered and analyzed
in SPSS version 19. For continuous variables (e.g.
SBP, DBP) means with standard deviations (SDs)
were reported. For dichotomous data, we calculated
proportions. Independent t-test was used to identify
the difference in mean BP level among intervention
and control groups. Chi-square test was applied
to observe effect of intervention on exercise
habits and medication adherence. Items within
each scale of PSQ 18 are averaged after scoring.
These scale scores represent the average for all
items in the scale that were answered. High scores
on PSQ 18 reflect satisfaction with medical care.
Intention to treat analysis was carried out for
all participants.
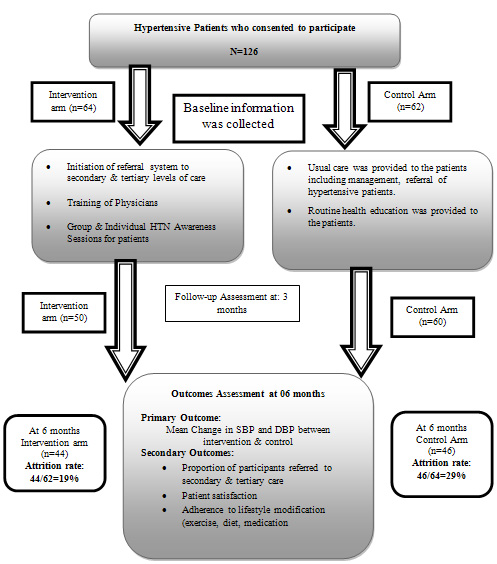
A total of 126 (intervention:
62, control: 64) patients were recruited at baseline,
out of which 90 patients (44 intervention group,
46 control group) completed the study protocol
and were included in the final analysis. The overall
attrition rate was 29% in the control group and
19% in the intervention group (Figure 1).
Figure 1: Flow of Study participants
The mean age of the participants in the intervention
group was 50.5+ 8.7 years and 52.0 +8.3 years
in the control group. The socio demographic characteristics
of study participants are given in Table 1. Both
the study groups had preponderance of female participants
(intervention: 61.4% v/s control: 69.6%). About
11% of the participants in the intervention group
and 8.7% in the control group were unable to read
or write. Over 80% of the participants in both
the groups had family history of hypertension.
Both the study groups were similar in terms of
the demographic characteristics such as age, gender,
educational status etc.
Table 1 : Descriptive Characteristics of Intervention
and Control Groups
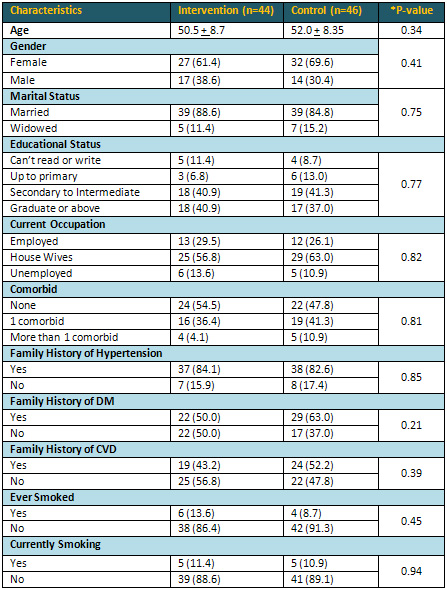
*P value=chi square P value, significance kept
at < 0.05
A statistically significant mean difference of
17.35 mm Hg was observed in systolic BP of intervention
(140.2 + 14.6 mm Hg) and control group (157.6
+ 17.5) after a follow-up of 06 months (Table
2). Likewise a 7 point difference was observed
in diastolic BP (intervention: 86.0 + 6.6). Changes
in blood markers of blood pressure control at
six months follow-up are presented in Table 2.
Table 2: Intervention and Control Groups at
baseline and six months follow-up
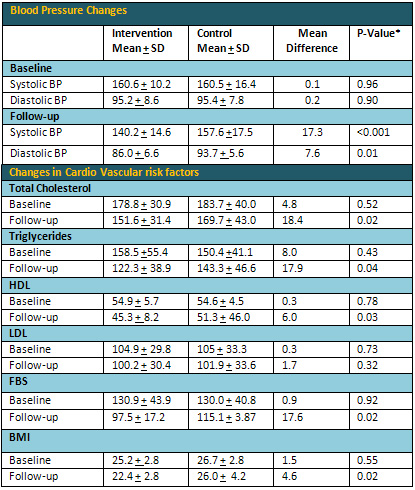
*P value=Two independent T-test P value, significance
kept at < 0.05
Satisfaction with services was assessed through
PSQ-18 scale which has seven dimensions. There
was a significant difference in the mean scores
of satisfaction levels between intervention (3.9
+ 0.2) and control groups (3.7 + 0.2) with a P-value
of 0.003 (Table 3).
Table 3: Participant's Satisfaction and Changes
in life style of study participants (n=90)
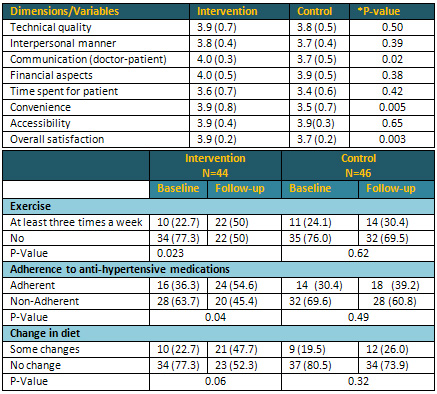
*P- Value for difference in satisfaction dimensions
by intervention & control group based on independent-T-test
*P value=chi square P value,
significance kept at < 0.05
The average monthly cost of hypertension treatment
was PKR.653 + 376 among the intervention and PKR.753
+ 817 in the control group. This difference however,
was not statistically significant (P=0.45).
The majority (54.6%) of the patients in the intervention
group were taking antihypertensive medications
regularly, in comparison to 39.2% of the patients
in the control group (P=0.001). About 50% of the
participants in the intervention group started
some level of exercise (at least thrice a week
for 30 minutes) after the intervention (Table
3).
The primary aim of this study
was to evaluate the effectiveness of strengthening
the health care delivery system in general and
primary care in particular to control epidemic
of hypertension. The program included patient
group education sessions regarding hypertension
and training of Family Physicians along with strengthening
of health care delivery system at primary, secondary
and tertiary levels. This study has found a favorable
impact on lowering Blood Pressure and can therefore
be implemented on a larger scale. This is consistent
with several similar intervention programs conducted
in various countries on varied populations.(10-13)
In this study, lifestyle changes including dietary
modification and physical exercise, along with
medication adherence, responded favorably to the
intervention. In the study, the mean reduction
in Systolic Blood Pressure (SBP) at six months
follow-up was 17.3 mmHg. The findings are consistent
with numerous studies where in community based/behavioral
intervention had achieved a difference of 15-20
points in the SBP.(14-19)
This study strengthened the referral
system in which the hypertensive patients are
managed in primary care settings, and referred
to secondary and tertiary care settings if the
patients are more challenging or develop complications.
In this study, none of the patients were referred
to secondary or tertiary care settings. This is
most likely because, the Family Physicians were
better trained to manage non-complicated cases.
Besides that, it can also be due to the fact that
patients didn't have hypertension for a longer
duration of time so the chances of developing
the complications were less; hence they were effectively
managed at the primary care level. An additional
reason could be small sample size.
In this study, Family Physicians were trained
based on latest guidelines to manage hypertension.
The group education sessions provided patients
with latest information on lifestyle modifications.
It is evident that regular visits of patients
allow doctors to monitor patients closely and
the physicians can encourage self-care among patients,
and it can help in better treatment adherence
and reduction in blood pressure.(17, 20)
Repeated reminder calls for medication adherence
and life style modifications have yielded the
desired results observed at six months interval.
Regular contact with physicians increases patients
comfort level with doctors. This is consistent
with our study wherein patients in the intervention
group had higher satisfaction scores than control.
It is reported that weight loss leads to blood
pressure reduction on a long term basis.(21) In
the current study; there was a significant improvement
in Body Mass Index (BMI) levels post intervention.
This adds to the favorable impact of weight management
in the current study on blood pressure control.
Lack of adherence to medications is the common
cause for uncontrolled hypertension. Prevalence
of non-adherence to hypertensive medication is
demonstrated to be a significant for lack of control
of blood pressure. (22) This study demonstrates
positive impact of intervention that improves
adherence to treatment with resultant favorable
outcome on blood pressure control.
Significant results were
observed in this study, however, the findings
of this study should be interpreted cautiously
as it was conducted in two study clinics located
at a reasonable distance to one another and with
less attrition rates observed as compared to other
community based intervention trials. Moreover,
the lack of blinding of patients and assessor
could have resulted in more impact of intervention;
as the patients in the intervention arm have received
the best possible treatment. Moreover, the follow-up
period of this study was only six months so we
were unable to determine the long-term sustainability
of BP and effect of the interventions on cardiovascular
outcomes. Despite these limitations, there is
evidence emerging from this pilot study that intervention
at primary care level along with strengthening
of the health care system results in better blood
pressure control among patients with hypertension.
Hypertension can be effectively
managed in the primary care setting through interventions
even in developing countries with weak primary
health care structure. Such intervention at primary
care level along with strengthening of the health
care system should be undertaken to better manage
hypertension.
Acknowledgement:
We are grateful to The Aga Khan University Research
Council, for providing a grant to conduct this
study. We are also grateful to the administration
of two study clinics for their cooperation during
the implementation of the study. We would also
like to thank all the patients for giving their
time to this project.
1. Temilolu Olayinka Aje, Michael
Miller. Cardiovascular disease: A global problem
extending into the developing world. World J Cardiol.
2009 Dec 31; 1(1): 3-10.
2. Ibrahim MM, Damasceno A. Hypertension in developing
countries. The Lancet. 2013; 380(9841):611-9.
3. Pereira M, Lunet N, Azevedo A, Barros H. Differences
in prevalence, awareness, treatment and control
of hypertension between developing and developed
countries. Journal of hypertension. 2009; 27(5):963-75.
4. Safdar NF, Bertone-Johnson ER, Cordeiro L,
Jafar TH4, Cohen NL. Dietary patterns and their
association with hypertension among Pakistani
urban adults. Asia Pac J Clin Nutr. 2015; 24(4):710-9
5. Ragot S, Beneteau M, Guillou-Bonnici F, Herpin
D. Prevalence and management of hypertensive patients
in clinical practice: Cross-sectional registry
in five countries outside the European Union.
Blood Pressure. 2016 Apr; 25(2):104-16.
6. Hashmi SK, Afridi MB, Abbas K, Sajwani RA,
Saleheen D, Frossard PM, et al. Factors associated
with adherence to anti-hypertensive treatment
in Pakistan. PLoS One. 2007; 2(3):e280.
7. Feng YJ, Wang HC, Li YC, Zhao WH. Hypertension
Screening and Follow-up Management by Primary
Health Care System among Chinese Population Aged
35 Years and above. Biomed Environ Sci. 2015 May;
28(5):330-40.
8. Jafar TH. Combined patient
and GP training best for BP control in Pakistan.
PharmacoEconomics & Outcomes News. 2011; 640:29.
9. Stallard P. Validity and reliability of the
Parent Satisfaction Questionnaire. British journal
of clinical psychology. 1996;35(2):311-8.
10. Rakotz MK, Ewigman BG, Sarav M, Ross RE, Robicsek
A, Konchak CW, et al. A technology-based quality
innovation to identify undiagnosed hypertension
among active primary care patients. The Annals
of Family Medicine. 2014; 12(4):352-8.
11. Look ARG. Long term effects of a lifestyle
intervention on weight and cardiovascular risk
factors in individuals with type 2 diabetes: four
year results of the Look AHEAD trial. Archives
of internal medicine. 2010; 170(17):1566.
12. Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante
JP, Isen AM, Jobe JB, et al. A randomized controlled
trial of positive-affect intervention and medication
adherence in hypertensive African Americans. Archives
of internal medicine. 2012; 172(4):322-6.
13. Stevens VJ, Corrigan SA, Obarzanek E, Bernauer
E, Cook NR, Hebert P, et al. Weight loss intervention
in phase 1 of the Trials of Hypertension Prevention.
Archives of internal medicine. 1993; 153(7):849-58.
14. Anchala R, Kaptoge S, Pant H, Di Angelantonio
E, Franco OH, Prabhakaran D. Evaluation of Effectiveness
and Cost-Effectiveness of a Clinical Decision
Support System in Managing Hypertension in Resource
Constrained Primary Health Care Settings: Results
From a Cluster Randomized Trial. Journal of the
American Heart Association. 2015; 4(1):e001213.
15. Appel LJ, Champagne CM, Harsha DW, Cooper
LS, Obarzanek E, Elmer PJ, et al. Effects of comprehensive
lifestyle modification on blood pressure control:
main results of the PREMIER clinical trial. JAMA:
Journal of the American Medical Association. JAMA.
2003; 289(16):2083-93 2003.
16. Bosworth HB, Olsen MK, Neary A, Orr M, Grubber
J, Svetkey L, et al. Take Control of Your Blood
Pressure (TCYB) study: a multifactorial tailored
behavioral and educational intervention for achieving
blood pressure control. Patient education and
counseling. 2008; 70(3):338-47.
17. Aziz KU. Evolution of systemic hypertension
in Pakistani population. Journal of the College
of Physicians and Surgeons--Pakistan: JCPSP. 2015;
25(4):286-91.
18. Hasandokht T, Farajzadegan Z, Siadat ZD, Paknahad
Z, Rajati F. Lifestyle interventions for hypertension
treatment among Iranian women in primary health-care
settings: Results of a randomized controlled trial.
Journal of research in medical sciences: the official
journal of Isfahan University of Medical Sciences.
2015; 20(1):54.
19. Margolis KL, Asche SE, Bergdall AR, Dehmer
SP, Maciosek MV, Nyboer RA, et al. A Successful
Multifaceted Trial to Improve Hypertension Control
in Primary Care: Why Did it Work? Journal of general
internal medicine. 2015:1-8.
20. Gwadry-Sridhar FH, Manias E, Lal L, Salas
M, Hughes DA, Ratzki-Leewing A, et al. Impact
of interventions on medication adherence and blood
pressure control in patients with essential hypertension:
a systematic review by the ISPOR medication adherence
and persistence special interest group. Value
in Health. 2013;16(5):863-71.
21. Stevens VJ, Obarzanek E, Cook NR, Lee IM,
Appel LJ, West DS, et al. Long-term weight loss
and changes in blood pressure: results of the
Trials of Hypertension Prevention phase II. Annals
of internal medicine. 2001; 134(1):1-11.
22. Raebel MA, Ellis JL, Carroll NM, Bayliss EA,
McGinnis B, Schroeder EB, et al. Characteristics
of patients with primary non-adherence to medications
for hypertension, diabetes, and lipid disorders.
Journal of general internal medicine. 2012; 27(1):57-64.
|