|
Early And Late
Outcome For Single Versus Double Stenting For
Bifurcational Coronary Artery Lesions
......................................................................................................................................................................
Aram J. Mirza
Correspondence:
Dr. Aram J. Mirza
Interventional Cardiologist
Director, Cathlab , Sulaimany Cardiac Hospital.
P.O. Box: 198, Sulsimany, Iraq
Email: arammerza@ymail.com
|
ABSTRACT
Objectives: The purpose of this study
is to evaluate two different techniques
of stent placement in bifurcation lesions
of coronary artery disease.
Background: Although stent placement
with dedicated techniques has been suggested
to be a useful therapeutic modality for
treating bifurcation lesions, limited information
is available if stent placement on the side
branch and on the parent branch provides
any advantage over a simpler strategy of
stenting the parent vessel and balloon angioplasty
of the side branch.
Methods: Between
January 2010 and January 2012, we treated
a total of 92 patients with bifurcation
lesions with two strategies, stenting the
parent vessel and balloon angioplasty of
the side branch (group A, n=70) or stenting
both vessels (group B, n=22). Angiograms
were analyzed by quantitative angiography,
and clinical follow-up was obtained for
six months.
Results: Stent placement
on both branches resulted in a lower residual
stenosis in the side branch. Acute procedural
success was similar in the two groups(100%).
At the six-months follow-up, the angiographic
restenosis rate and the target lesion revascularization
rate were similar in the two groups, but
repeated percutaneous coronary intervention
done for symptomatic patients with denovo
lesions in other arteries. There was no
difference in the incidence of six-months
total MACE.
Conclusions: For
the treatment of true bifurcation lesions,
a complex strategy of stenting both vessels
provided no advantage in terms of procedural
success and late outcome versus a simpler
strategy of stenting only the parent vessel.
Key words:
Stent, Bifurcational, coronary arteries.
|
Among complex coronary lesions,
bifurcations are those most frequently encountered
by every interventional cardiologist. Bifurcation
complexity essentially relies on their specific
anatomic configuration, which is imperfectly handled
by current coronary devices.
Anatomy of Bifurcation Lesions
A coronary bifurcation
is a branching artery constituted by a main vessel
(MV) and a side branch (SB). The segment before
the origin of the SB is referred to as proximal
MV, whereas the one that is distal to it is referred
to as distal MV. The tissue membrane separating
the origins of the 2 bifurcation arms is called
the flow divider or carina.
Operative definitions of bifurcation lesions have
been based on the SB diameter, either arbitrarily
or in relation to potential blood supply.
Actually, a bifurcation stenosis is defined as
a coronary artery narrowing occurring adjacent
to and/or involving the origin of a significant
SB (3). To be significant the SB has to be considered
important in the individual patient according
to symptoms, location of ischemia, vitality, collateral
vessels, and left ventricular function.
Morphology classification is mainly based on plaque
distribution. Indeed, plaque distribution can
variably involve the proximal MV, the distal MV,
or the SB. This has engendered at least 6 different
classification schemes (1,3).
Sometimes, branching arteries are called "true"
rather than "false" bifurcations according
to the mere presence or absence of significant
SB stenosis.
Pathological examination (4,5) of coronary arteries
reveals that the atherosclerotic plaques are mainly
located in areas of low shear stress, such as
the lateral walls of the MV and SB, whereas they
are less common at the carina level, which is
characterized by high shear stress.
The spatial relation between the 2 arms of the
bifurcation can be defined by 3 angles that have
been recently named A (the angle between the proximal
MV and the SB), B (the angle between the SB and
the distal MV), and C (the angle between the proximal
and distal segment of the MV). At times, bifurcations
are defined as V- or T-type according to angle
B being < 70° or > 70°, respectively.
Moreover, the proximal and distal branches of
a bifurcation often do not lie on a single plane,
thus posing significant challenges to quantitative
coronary angiography software.
A recent ex vivo study of polymer casts of human
coronary arteries has revealed a complex curvilinear
transition zone between MV and SB, mainly characterized
by an elliptical and asymmetrical configuration
of the SB ostium and brief tapering of the SB
origin (2,3).
Moreover, it has been previously pointed out that
SB ostium asymmetry increases with increasing
bifurcation angles. In bifurcations, there is
also an asymmetrical geometric reduction according
to the law of conservation of energy (2,3).
The complex interaction among different factors
makes every bifurcation lesion quite unique (Fig.
7), although certain lesion characteristics have
been associated with treatment success when using
currently accepted techniques and DES platforms
(5,6)
The treatment of stenoses at a bifurcation remains
one of the most challenging lesion subsets in
coronary angioplasty.
Bifurcation lesions carry a risk of side branch
occlusion because of plaque redistribution or
so-called "plaque shift" across the
carina of the bifurcation. The risk is increased
if there is an eccentric lesion at the bifurcation
site and a stenosis in the ostium of the side
branch (7,8,9).
To lower the risk of plaque shift, the "kissing"
balloon technique was developed (2). However,
the results after balloon dilatation of bifurcation
lesions are frequently suboptimal with a high
incidence of complications and restenosis(7,8,9).
It has also been pointed out that optimal results
and low complication rates could not necessarily
be anticipated by all operators (8).
The use of coronary stents has improved the treatment
of bifurcation lesions, but they are technically
challenging and there is compromising of the branch
vessel (10,11,12).
Stent implantation on both the parent vessel and
the side branch, which is called "kissing
stents," is a useful technique for maintaining
maximum expansion of both vessels(12,13).
The use of two stents minimizes lumen loss of
one side during expansion of the other vessel
(12).
The six main techniques used for bifurcation stenting
(the "T" stent and modified "T"
stenting, the "V" stent, the 'Y"
stent, crush technique and the "Culotte"
technique) have been shown by figures 1, 2, 3,
4, 5 and 6 (13,14).
Although these dedicated techniques have evolved
along with new stent designs, it is not clear
if the strategy of stenting both vessels provides
better outcome than that of stenting only the
parent vessel. So far, only case reports or limited
series are available to understand the results
of these different techniques(10,11,12,13,14,15).
For this reason, we analyzed in-hospital results
and long-term outcomes for 92 consecutive patients
with true bifurcation lesions treated with either
stenting both vessels or stenting the parent vessel
plus balloon angioplasty for the branch and we
use Madina classification in our description and
management of bifurcational lesions.
Until the advent of drug-eluting stents (DES)
and dedicated techniques, percutaneous bifurcation
interventions were associated with very high rates
of unfavorable outcomes (12,13,14). Nevertheless,
procedures directed to bifurcation treatment are
often technically demanding and require proper
execution. When implementing dedicated percutaneous
bifurcation approaches, kissing balloon (KB) has
been variably recommended to optimize stent apposition,
correct stent deformation or distortion and improve
side branch (SB) access. Over the years, KB has
been deeply investigated by many different methods,
from bench testing and computer simulations to
in vivo intravascular imaging and clinical studies
that have produced a large amount of data.
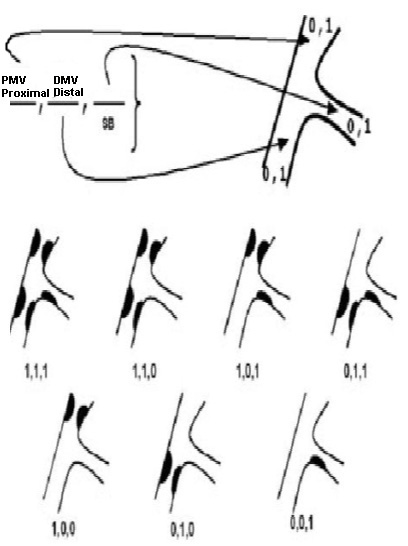
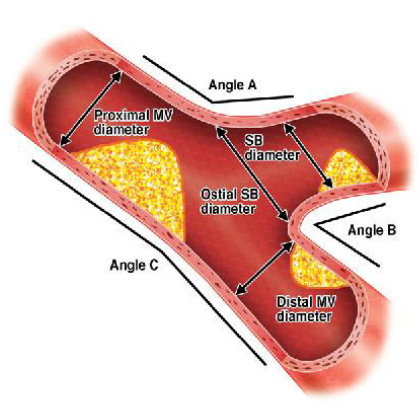
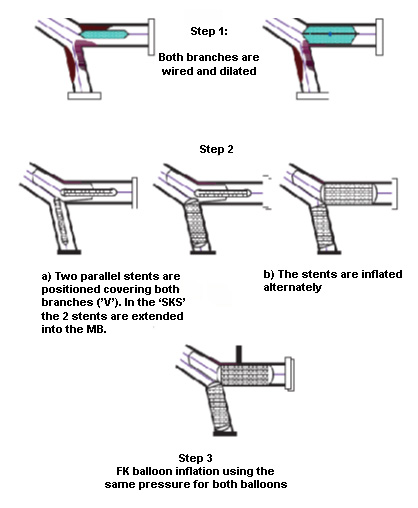
Figure 1: The "V" and "simultaneous
kissing stents" (SKS) stenting technique.
FK - final kissing; MB - main branch
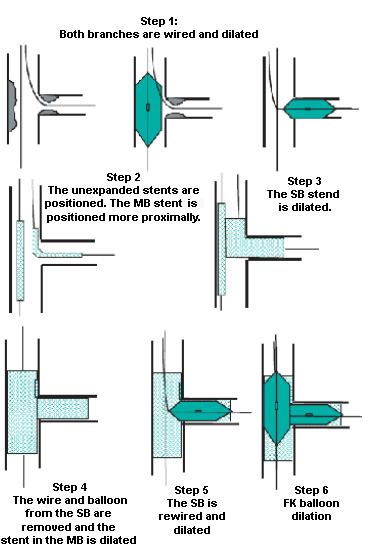
Figure 2: "Crush" technique. FK -
final kissing; MB - main branch; SB - side
branch.
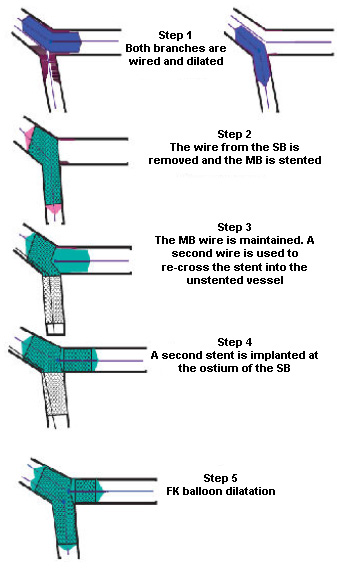
Figure 3: The T stenting technique (through
the stent). FK - final kissing; MB - main branch;
SB - side branch
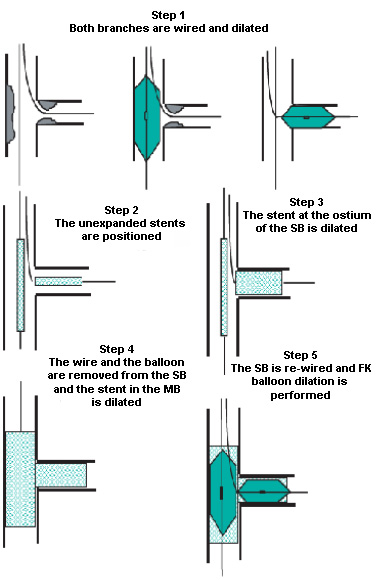
Figure 4: The modified "T" stenting
technique. FK - final kissing; MB - main
branch; SB - side branch
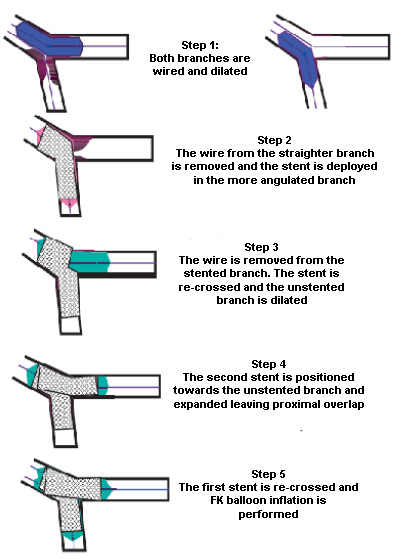
Figure 5: The "cullottes" stenting
technique. FK - final kissing

Figure 6: The "Y" stenting technique.
FK - final kissing
Study Population
The study was done retrospectively and prospectively
between January 2010 and January 2012. A total
of 92 patients underwent coronary stenting at
Sulimaniya Center For Heart Disease for the treatment
of symptomatic bifurcation lesions that had a
>50% diameter stenosis in both the parent vessel
and the ostium of the contiguous side branch and
the lesions confirmed by two interventional cardiologists.
Informed consent for coronary angiography and
stent implantation was obtained from all patients.
Revascularization Procedure and Stenting Strategies
Before angioplasty, the patient was on maintenance
dose of oral aspirin with clopidogrel loading
dose (600mg) given a day before the intervention
and intravenous bolus of heparin (70-100Unit/kg)
were administered to all patients
at time of intervention.
Angiograms in multiple views were obtained using
the transfemoral approach.
After placement of the guiding catheter, two wires
were inserted in the distal bed of the two branches.
Balloon angioplasty was conducted by sequential
inflation of a semicompliant balloon in each branch.
Two strategies for bifurcations
were available
A less complicated angioplasty strategy that used
stenting in only the parent vessel of the bifurcation
lesions (group A) and a more complicated angioplasty
treatment strategy that included stenting of both
branches of bifurcation lesion (group B) was undertaken.
As a general rule, both lesions were stented when
the reference vessel size of the side branch was
greater than 2.0 mm. Group A was comprised of
70 patients and Group B was comprised of 22 patients.
For group A, the stent was implanted in the parent
vessel and then balloon dilatation was performed
through the stent struts into the side branch.
Simultaneous kissing balloon inflation was frequently
performed on completion of the procedure. For
group B, stent placement for both vessels was
performed using one of the previously reported
techniques (Figures1,2,3,4,5,&6).
Angiographic Analysis and
Clinical Follow-up
We used a computer-based QCA-CMS system version
4.0 for quantitative coronary angiography (QCA),
with the dye-filled catheter as a reference. Reference
diameter, lesion length and minimum luminal diameter
(MLD) were measured before and after angioplasty,
and at the time of follow-up angiography.
The diameter of the normal segment proximal to
the traced area in the parent vessel was used
to determine the parent vessel diameter, and the
side branch reference diameter was determined
from the diameter of the traced segment in the
normal segment distal to the lesion in the branch.
Lesion length was defined as the distance from
the proximal to the distal shoulder of the lesion.
Angiographic success was defined as post-PCI percent
diameter stenosis less than 20% with at least
Thrombolysis in Myocardial Infarction (TIMI) flow
3 in both the parent vessel and side branch. Procedural
success was defined as the achievement of angiographic
success in the absence of any in hospital major
adverse cardiac events (MACE), which include death,
myocardial infarction (MI) or emergency percutaneous
treatment or coronary artery bypass grafting (CABG).
Emergency coronary bypass surgery was defined
as bypass surgery involving immediate transfer
of the patient from catheterization laboratory
to the operating room or within 24 hours of the
procedure.
Follow-up angiography was planned for all patients
at six months or earlier, if there was a clinical
indication.
Restenosis was defined as .50% diameter stenosis
of the treated lesion.
Clinical follow-up was obtained around six months
after treatment by direct patient interview.
Target lesion revascularization (TLR) was defined
as any repeat percutaneous intervention to the
target lesion (parent or side branch) or any coronary
bypass graft to the treated vessel during follow-up.
Six-month total MACE was defined as death, MI
or target lesion revascularization during the
follow -up period, plus in-hospital MACE.
Statistical Analysis
Data are expressed as mean
SD for continuous variables, as numbers with percentage
for categorical variables. Continuous data were
compared using unpaired Student t test, and frequencies
were compared using the chi-square or Fisher's
exact test. A p value of 0.05 was considered statistically
significant.
Table 1: Baseline clinical
characteristics
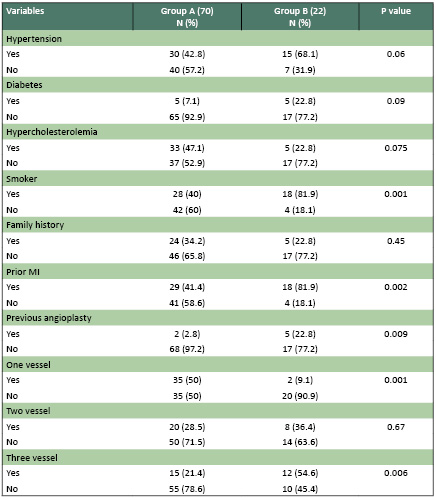
Between group A and
group B, there was no difference in baseline clinical
characteristics except for the extent of coronary
artery disease or the location of bifurcation
lesion; more patients with one vessel disease
were included in group A and more patients with
two vessel disease were included in group B.
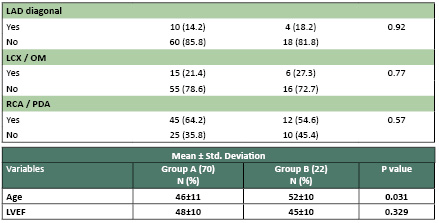
Table 2: Baseline angiographic characteristics
Baseline angiography characteristics
of the parent vessel were similar in both groups.
For side branch the vessel size and lesion length
were greater in group B than Group A(3.5+_0.5
vs 2.0+_0.5 ,p 0.140 ; 20.0+_10.0 vs 10.0 +_0.5
p 0.001).
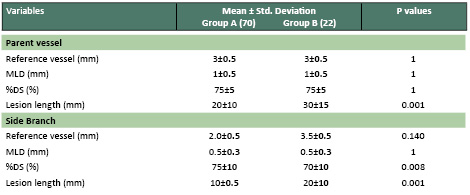
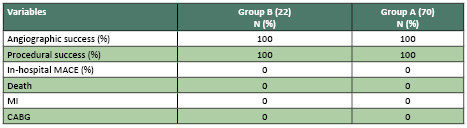
Table 3: Procedural
characteristics
In group B, the modified T technique
and crush technique was used in the majority of
patients. The procedure for Group B needed more
stents (2-3) and longer time than Group A (60+_15
vs, 45+_15, p=0.001). The total stent length per
patient was longer in Group B than Group A (38+_15
vs.38+_10,p=1). The final balloon/vessel ratio
was similar in the two groups. Higher inflation
pressure was applied in group B than in group
A for both the parent vessel and the side branch
(16+_4 vs.13+_3 p=0.07: 10+_4 vs.8+_4 p=0.07).
All procedures were completed with simultaneous
kissing balloon inflation in group A and B.
Table 4: Angiographic and clinical follow-up
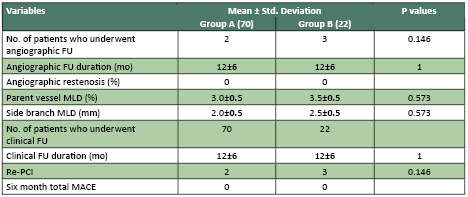
The angiographic follow-up
rate for group A and group B were only done for
those who were symptomatic (2 of group A and 3
of group B) and where there was found lesions
in other arteries not the target artery that stented.
Follow-up QCA measurements of the parent vessel
were larger in group B (3.5+_0.5 vs.3.0+_0.5 p=0.573).
Patients of group B had side branches with a larger
reference vessel size compared with patients of
group A (2.5+_o.5 vs.2.0+_0.5 p=0.573). There
was no difference between the two groups in the
MLD. The angiographic restenosis rate was (0%)
for patients in group B and (0%) for those in
Group A. Clinical follow-up was accomplished in
all patients.
The TLR rate was similar in the two groups (0%).
Six-month total MACE, including TLR was similar
in the two groups.
The optimal
strategy for percutaneous treatment of bifurcation
lesions is one of the most widely debated issues
in interventional cardiology.
To date, available data suggest that, in clinical
practice, single stent implantation, when feasible,
is not inferior to double stenting techniques.
However, it is also well established that a remarkable
proportion of treated lesions may require double
stenting to obtain angiographic success.
The relevance of the involvement of atherosclerosis
in bifurcation lesions is underlined by the existence
of a number of attempts to categorize these lesions,
including the Duke, the Sanborn, the Safian, the
ICPS, and the Medina classifications. Among these,
the Medina classification is considered the most
simple and has recently been recognized in a consensus
report by European experts as the gold standard
for bifurcation evaluation.
The best classification, however, should not only
provide a simple description of the anatomy but
should also help in selecting the appropriate
stent implantation strategy.
Taking these assumptions as a starting point,
we used the Medina classification prospectively
in a consecutive series of patients with bifurcation
lesions undergoing PCI in order to assign them
to a single or double stenting strategy.
In our study, the angiographic results obtained
in MV and SB with a single stent in group A did
not differ from that obtained with 2 stents in
the group B patients. Similar results have been
obtained in other studies (7,8,9,10,11,18) in
which double stenting of bifurcation lesions is
not advantageous and seems also to have a detrimental
impact on major clinical outcomes.
On the other hand, the selection of double stenting
techniques in patients with the more complex Medina
1,1,1 lesions resulted in a high rate of angiographic
success and warranted, over the long term, a clinical
outcome that was comparable to that observed in
patients with less complex bifurcations treated
with single stenting.
The selection of Medina 1,1,1 further restricted
the number of patients considered for double stenting
in the present study compared to the classical
definition of "true bifurcation" which
also comprises Medina 1,0,1 and Medina 0,1,1 lesions.
The latter lesions were successfully managed with
a single stent in the present study. Moreover,
some patients with Medina 1,1,1 lesions may be
treated by single stenting due to the presence
of a SB anatomy that is not ideal for a second
stent implantation (diffuse disease with absence
of an appropriate stent landing zone, distal SB
occlusion, presence of further division of the
SB in multiple distal branches, etc).
Observational studies (8,9,10) have shown that
up to 90% of jailed side branches are usually
clinically silent and probably do not affect long-term
clinical event-free survival and this may explain
why most of the patients are asymptomatic even
with jailed SB.
All together, these observations support the concept
that only a minority of bifurcation lesions should
be considered for double stent implantation techniques.
Finally, as previously shown by other studies
(9,10) DES implantation seems to be necessary
to treat bifurcation lesions as it is associated
with a lower TLR rate and is an independent predictor
of better clinical outcome as compared to BMS.
Study Limitations
1- In this study,
we have arbitrarily hypothesized that the use
of double stenting techniques may be reserved
to treat Medina 1,1,1 lesions. This assumption
has not been previously well established and remains
controversial.
2- The failure to use dedicated software
for the quantitative analysis of bifurcation lesions
and the lack of systematic angiographic follow-up
represent important limitations in the comparison
of the acute angiographic results and the long-term
outcome.
1- The selection of a
single stenting strategy based on the absence
of Medina 1,1,1 lesions is associated with a high
rate of optimal angiographic results and with
a low rate of bailout SB stenting.
2- The selection of a double stenting strategy
only in patients with Medina 1,1,1 lesions is
associated with a high rate of optimal angiographic
results.
3- Both stenting strategies selected on
the basis of the Medina classification are associated
with a low rate of MACE.
4- In the absence of randomized trials,
our observational study might help in the selection
of a personalized stenting strategy for bifurcation
lesions.
Recommendations
1- For treatment of bifurcation lesions
a complex strategy of stenting both vessels provides
no advantage in terms of procedural success and
late outcome versus simple strategy of stenting
only the parent vessel.
2- Double stenting of both main vessel
and the side branch vessel in bifurcation lesion
could be considered in cases of very big bifurcation
branch, such as main stem lesions or lesions involving
bifurcation branches with diameter almost as big
as that of the main branch or jeopardization of
the side branch with TIMI flow less than three.
Abbreviations and Acronyms
CABG = Coronary artery bypass graft surgery
DCA = Directional coronary atherectomy
MACE = Major adverse cardiac events.
MI = Myocardial infarction
MLD = Minimum luminal diameter
QCA = Quantitative coronary angiography
TIMI = Thrombolysis in myocardial infarction
TLR = Target lesion revascularization
LMS = Left main stem.
LAD = Left anterior descending artery.
LCX. = Left circumflex artery.
RCA = Right coronary artery
PDA = Posterior descending artery.
D1 = First Diagonal.
OM = Obtuse marginal.
DS% = Percent diameter stenosis.
LVEF = Left ventricular ejection fraction.
SD = Standard deviation.
FU = Follow up.
PCI = Percutaneous coronary intervention.
SB = Side branch.
MV = Main vessel.
1- Daniel Todaro, Francesco Burzotta,
Carlo Trani, et al. Evaluation of a Strategy for
Treating Bifurcated Lesions by Single or Double
Stenting Based on the Medina Classification, Rev
Esp Cardiol,2009;62(6):606- 14.
2- Gregory A. Sgueglia, Bernard Chevalier, Latina,
Italy; and Massy, France Kissing Balloon Inflation
in Percutaneous Coronary Interventions J A C C
: C A R D I O V A S C U L A R I N T E R V E N
T I O N S V O L . 5 , N O . 8 , 2 0 1 2.
3- Georgios Sianon; Marie-Angèle More;
Arie Pieter Kappetein. The
SYNTAX Score: an angiographic tool grading the
complexity of coronary artery disease EuroInterv.2005;1:219-227
4- Gaku Nakawaza, Saami K, Y Zadani, Aloki V Finn.
Pathological Findings at Bifurcational lesions,
jack journals, April 2010. volume 55, Issue 16,
5- Nakawaz G, Yazdani SK, Vorpahi M, Kolodgie
FD. Pathological Findings at Bifurcational lesions:
The impact of flow distribution on atherosclerosis
and arterial healing after stent implantation
,J Am Coll Cardiol 2010 april 20;55:1679-8
6- IOANNIS IAKOVOU, ANTONIO COLOMBO Centro Cuore
Columbus and San Raffaele Hospital, Milan, Italy
Two-Stent Techniques for the Treatment of Coronary
Bifurcations with Drug-Eluting Stents Hell J Cardiol
,2005 ,46: 188-198,.
7- Jassim AL Suwaidi; Peter Berger, Chraranjit
S Rihal ,Kirk N Garratt. Immediate and long term
out come of intra coronary stent implantation
for true bifurcational lesions. J Am Coll Cardiol
,2000;35 (4); 929-936.doi;10.1016/S0735-1097(99)00648-8.
8- Katritsis DG, Siontis GC, Ioannidis JP et al.
Double versus single stenting for coronary bifurcation
lesions: a meta analysis, circinterventions, ahajournals.org
by guest on april 25,2013-
9- Takehiro Yamashita, Takahiro Nishida, Milena
G. Adamian, , Carlo Briguori, Marco Vaghetti,
Nicola Corvaja, Remo Bifurcation Lesions: Two
Stents Versus One Stent Immediate and Follow-up
Results Journal of the American College of Cardiology,
20005 Vol. 35, No.
10- Takehiro Yamashita, Nicola Corvaja Remo Albero.
Bifurcational lesions: Two stent versus one stent
- immediate and follow up results, J Am Coll Cardiol
;2000;35(5); 1145 1151,dio;10,1016/S0735-1097.
11- Keiichi Tsuchida, Antonio Colombo, Theirrey
Lefevere. The clinical outcome of percutaneous
treatment of bifurcation lesions; European Heart
Journal (2007 )28 ,433-442.
12- Erik Jorgensen and Steffen Heiqvist. Stent
treatment of coronary artery bifurcation lesions;
European Heart Journal;(2007)28,383-385.
13- Ioannis Iakovou. Contemporary Stent Treatment
of Coronary Bifurcations HOSPITAL CHRONICLES 2006,
SUPPLEMENT: 110-114.
14- Azeem Latib and Antonio Colombo. Management
of bifurcational lesions; Interventional cardiology
unit Ssn Raffaele Scientific Institute, Milano,
Italy, Via Buonarroti 2004, 48, 20145.
15- Angela Hoye,Ionnis Lakovou; Lei Ge,. Long
term outcomes after stenting bifurcation lesions
with Crush Technique; Jacc Journal, May 2006 Volume
47,Issue 10.
16- Yves Louvard, Martyn Thomas, Vladimir Dzavik.
Classification of coronary bifurcation lesions
and treatment; catheterization and cardiovascular
interventions (2008) 71; 175-183.
17- Aron V. Kaplan. Percutaneous coronary intervention
Treatment of bifurcation lesions; J Am Coll Cardiol
2009;195-196,doi;jcin 2009.01.003.
18- Andrejs Erglis; Indulis Kaumsars; Matti Niemela
; Randomised comparison of coronary stenting with
crush versus the culotte technique using sirolimus
eluting stent; Cardiovascular intervention ,2009;2;27-34.
19- Keiichi T Suchida, Antonio Colombo, Thierry
Lefever. Stent treatment of coronary artery bifurcation
lesions; European Heart Journal (2007)doi;10.1093.
20- Y.Louvard. ICPS, Massy, France; One stent
or two stents in coronary bifurcations: Athappan,
J Cardiovascular med 2010,11:103-110.
|