|
Cutaneous Leishmania
in Wadi Hadramout, Yemen
......................................................................................................................................................................
Amer Omer Bin Al-Zou
Correspondence:
Dr. Amer Omer Bin Al-Zou
Assistant Professor,
Department of Dermatology,
Faculty of Medicine
University of Aden
Yemen
Email: amer_zou2009@yahoo.com
|
ABSTRACT
Background: Cutaneous
leishmaniasis is widespread in Yemen, but
its extent has not been documented fully.
Objectives: The
objective was to describe epidemiological
and clinical features of cutaneous leishmana
cases.
Methods: It was a retrospective descriptive
records review of all patients with cutaneous
leishmaniasis diagnosed at the Seiyun general
hospital from January to December 2013.
Results: A total of 122 patients
were diagnosed with cutaneous leishmaniasis.
They were 73 (59.8%) males and 49 (40.2%)
females with the ratio male to female 1.5:1.
The age of patients ranged between 1 to
62 years and the mean age is 26.5 ±
18.1 years.
Most of the patients 56(45.9%) were of age
group less than 20 years.
The most common type of lesions were nodulo-ulcerated
52(42.7%) followed by nodular 45(36.9%).
The distribution of sex, in which males
and females of age group less than 20 years,
were predominant 38 (31.1%) and 18 (14.8%)
respectively.
The rest of the patients, males and females,
were convergent (p >0.05).
The majority of lesions' site were lower
limb 63 (51.6%) and the single lesions were
predominant 76 (62.3%) also, the most lesion
sizes were 0.5 cm 67 (54.9%) and 1 cm 50
(41%). Skin smears were positive in 102
(83.6%), negative in 9 (7.4%) and not done
in 11 (9.0%) patients.
Conclusion: We concluded that Wadi
Hadramout is an endemic region of leishmaniasis
and our findings will be of great interest
to the public health authorities in Hadramout.
Key words: Cutaneous
Leishmania, Wadi Hadramout, Yemen
|
Leishmaniasis is a parasitic
disease caused by more than 20 species of protozoa
of the genus Leishmania. It is transmitted by
the bite of female sandflies of the genera Phlebotomus
(Old World) and Lutzomyia (New World).
Pets and wild animals are the usual reservoir
and source of the infection (zoonotic transmission),
although the disease can also spread from human
to human (anthroponotic transmission). The disease
is endemic in more than 80 countries in Latin
America, Asia, Africa, and Southern Europe (1).
Other published literatures reported that Leishmaniasis
is endemic in 88 countries with incidence rate
of 1.5-2 million; the most common form of leishmaniasis
is cutaneous leishmaniasis (CL) with 1.5 million
new cases per year (2,3).
90% of cutaneous leishmaniasis are reported from
Iran, Afghanistan, Algeria, Iraq, Saudi Arabia,
and Syria in the Old World; and Bolivia, Brazil,
Colombia, and Peru in the New World (4).
Yemen is a tropical country, poor, has lack of
health care, and most of the population below
the poverty line (5).
There are very few reports on leishmaniasis in
Yemen in the international literature. Even though
it is not well documented, the disease seems to
be endemic in the country, and is primarily widespread
in arid and semiarid areas. It is also endemic
in the plateau and mountainous areas of Hadramout
governorate (5).
Hadramout governorate lies in the eastern part
of Yemen. The governorate comprises different
topography distributed between coastal plains,
mountains and hills of heights reaching 2000 m
above sea level, large areas of Al-Ruba Al-khali
desert, with many valleys; the largest Hadramout
valley which is supplied by many branch valleys,
is the longest valley and the most fertile in
the Arab peninsula since it is 160km long and
pours in Sihout on the Arab sea at Al-Mahra governorate.
The climate in Hadramout is a hot tropical climate.
Hadramout valley is considered one of the highest
valleys in technology related to water courses
drainage, as ducts water drainage are made within
hours, which is not usual in many large valleys
in Yemen where water courses continue running
for a long time. Seiyun city located 322km from
Mukalla, is the largest city in Hadramout valley
and it is the administrative capital of the valley
(6).
Figure 1: Cutaneous leishmaniasis
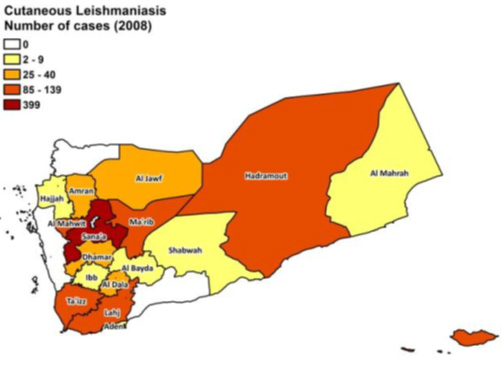
Source: YEMEN BASIC COUNTRY DATA Total
Population: 24,052,514 ...
www.who.int/leishmaniasis/.../YEMEN.pdf
To describe epidemiological
and clinical features of cutaneous leishmania
cases identified recently in Seiyun district,
Hadramout, Yemen.
Study area:
The study was conducted in Seiyun general hospital
which is the central hospital of Hadramout valley
and located in Seiyun city, Hadramaut, Yemen.
The hospital is a tertiary health institution
that renders medical care to its host community
and environs.
It serves as a referral center for neighbouring
areas which include cities of Hadramaut valley
and the surrounding villages.
Figure 2: The geographical
location of Hadramout valley (Wadi Hadramout)

Source: http://www.istockphoto.com/photos/wadi-hadramout?sort=best&excludenudity=true&mediatype=photography&phrase=wadi%20hadramout
Study period
This study was performed during the period January
to December 2013.
Study Design
A retrospective descriptive
records review was conducted.
Study sample:
The study population consisted of all patients
with cutaneous leishmaniasis diagnosed at the
Seiyun general hospital from January 2013 to December
2013.
The diagnoses were made by consultant dermatologist,
after reviewing the history, physical signs, clinical
pictures and clinical investigations of the patients.
Permission was sought and obtained in writing
from the director of the hospital and the head
of the medical records department of the hospital
to collect data from patient's case notes at the
medical records center.
Data collection procedure:
Checklist was prepared for collection of data
from patient record.
Data variables:
Data that were collected included the sex, age,
type of lesion, site of lesion, number of lesions,
size, result of skin smear and histopathology
in few cases (when needed).
Data Analysis and Presentation:
The data was analyzed and tabulated through descriptive
statistics using Microsoft Excel spreadsheet and
SPSS version 17 statistical software.
In the study year 2013, a total
of 122 patients were diagnosed with cutaneous
leishmaniasis according to their medical records.
They were 73 (59.8%) males and 49 (40.2%) females
with the ratio male to female 1.5:1.
The age of patients ranged between 1 to 62 years.
The mean age of the patients is 26.5 ±
18.1 years.
Most of the patients 56 (45.9%) were of age group
less than 20 years followed by the age group 40
years and more 35 (28.7%).
The most common type of lesions were nodulo-ulcerated
52 (42.7%) followed by nodular 45 (36.9%), papulo-nodular
17 (13.8%), plaque 5 (4.1%)
and ulcerated lesions 3 (2.5%) as shown in Table1
and Figures 3 to Figure 6.
Table 1: Variables of sex
and Types of lesions (n = 122)
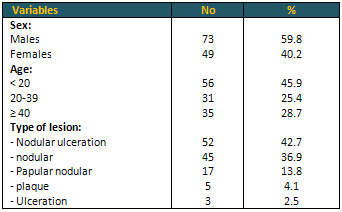
Figure 3: Nodular-ulcerated lesion on nose

Figure 4: Nodular lesion on nose
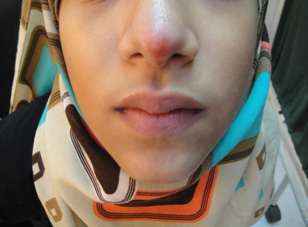
Figure 5: Ulcerated on lower limb

Figure 6: Multiple lesions on upper limb

Table 2 reveals the distribution of sex among
the study patients in which males and females
of age group less than 20 years were predominant
38 (31.1%) and 18 (14.8%) respectively. The rest
of the patients, males and females, were convergent.
The difference between values was not statistically
significant.
Table 2: Distribution of sex related to age groups
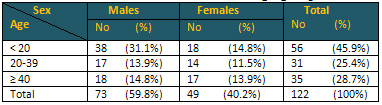
Calculation of percentage
out of the total patients 122
P > 0.05
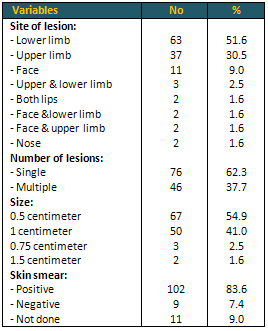
In Table 3 most of the lesions'
sites were lower limb 63 (51.6%) followed by upper
limb 37 (30.5%) and face (9.0%). The single lesions
were predominant 76 (62.3%) while multiple lesions
were 46 (37.7%). The majority of lesion sizes
were 0.5 cm 67 (54.9%) and 1 cm 50 (41%). Skin
smear was positive in 102 (83.6%), negative in
9 (7.4%) and not done in 11 (9.0%) patients.
Table 3: Characteristics of
cutaneous lesions among study patients (n = 122)
Leishmaniasis is a worldwide
disease (7,8,9). The World Health Organization
(WHO) estimates approximately 1 to 2 million new
cases of leishmaniasis each year, all over the
world (7,10). Twenty Leishmania species are pathogenic
for humans and 30 sand-fly species are proven
vectors (8). There are two main epidemiological
entities (8); zoonotic: where animal reservoir
hosts are involved in the transmission cycle and
Anthroponotic: where man is the sole reservoir
and only source of infection for the vector (8,11,12).
In the present study we found 122 patients were
diagnosed with cutaneous leishmaniasis and males
were significantly more affected than females;
they were 73 (59.8%) males and 49 (40.2%) females
with the ratio male to female 1.5:1. However,
in a study that was conducted in southeastern
France (13), males and females were equally affected
with cutaneous leishmaniasis. Other studies in
North-central province of Sri Lanka (14), in Lorestan,
Iran (15) and Al-Badarna, Libya (16) have shown
similar findings to our results.
This sex difference can be attributed to the following:
a) most of the residents of Wadi Hadramout are
farmers working on farms and they are at risk
of sandfly bites. Males are more active in the
palm plantations and harvesting dates, they are
more prone to sandfly bites.
In our study the age of patients ranged between
1 to 62 years. The mean age of the patients is
26.5 ± 18.1 years and the highest numbers
of patients 56 (45.9%) were less than 20 years
of age, which is similar to that reported by others
(17,18).
In contrast, Sharma et al (19) found a higher
incidence of cutaneous leishmaniasis in persons
21-30 years of age. As age increased, the number
of patients decreased; this finding may be caused
by acquired immunity.
The present study found that most lesions' sites
were lower limb 63 (51.6%) followed by upper limb
37 (30.5%) and face (9.0%). Similar findings were
reported by Syed et al (20) from Pakistan that
75% of the patients had lesions on the legs and
feet.
The study results of Khatri et al (21) from northwestern
Yemen varied to our findings. They reported that
the lesions were located on the face in 120 (88%)
patients, upper extremities in 31 (23%), lower
extremities in 17 (12.5%) and neck in one patient.
Also, Al-Qubati (22) mentioned that most lesions
occur in the head region, most commonly nose,
cheeks, and lips, with about 30% noted on the
extremities and a few on the trunk.
Aara et al (17) from India mentioned that the
most lesions were located on exposed parts of
the body such as the face (33%), upper extremities
(41%), and lower extremities (20%).The trunk was
involved in only 2% of patients.
Al-Nahhas et al (23) from Syria mentioned that
the lesions were mainly located on the upper extremities
(67.5%) compared with 25.9% on the facial region
and 6.5% on the legs, typical exposed fly bites
areas.
This variation of CL lesions location may be due
to the exposure of these two sites to the environments
more than the other site of the body and to the
direct contact with animals and soil because of
the traditional clothes of males in Valley Hadramout,
which make the lower limbs uncovered.
The majority of lesion sizes in our study were
0.5 cm 67 (54.9%) and 1 cm 50 (41%) which is smaller
than that reported in a previous study in northwestern
Yemen which reported that the size of the lesions
varied from 0.5 to 8 cm (21).
Also, it was smaller than that reported by Aara
et al (17) that Lesions varied in size from a
few millimeters to 12 cm in diameter and they
found a total of 1,938 (71%) of 2,730 lesions
ranged in size between 0.5 cm and 3.0 cm, and
only 48 lesions were > 5.0 cm.
Similar to our finding was that reported by Aguado
et al (24) from Spain that the most common lesion
size in their study was 0.5 cm followed by 1 cm.
In our study the single lesions were predominant
76 (62.3) while multiple lesions were 46 (37.7%),
similar to the results found by Khatri et al (21)
in which eighty-seven (64%) patients had a single
lesion, and the rest had multiple lesions. Also,
a study finding from Iran reported that the number
of lesions was one lesion in (67.7%) of the patients
and (32.3%) multiple lesions (15).
Khatri et al (21) mentioned that the types of
lesion were: nodulo-ulcerative, 75 (55%); ulcerated
plaques, 31 (23%); plaques, 19 (14%); nodular,
5; papular, 2; diffuse infiltration, diffuse infiltration
with ulceration, and verrucous thick plaques,
1 each.
The results of the current study revealed that
the most common type of lesions were nodulo-ulcerated
52 (42.7%) followed by nodular 45 (36.9%), papulo-nodular
17(13.8%), plaque 5(4.1%) and ulcerated lesions
3(2.5%).
To some extent the results were consistent with
previous studies from northwestern Yemen (21)
and from Turkey (25). Skin smears were positive
in 102 (83.6%), negative in 9 (7.4%) and not done
in 11 (9.0%) patients.
We carried out this study in
an attempt to compile cutaneous leishmania frequency,
types and site locations in patients who attended
to Seiyun hospital.
Males were more than females.
The results illustrated that male and female patients
of the age less than 20 years are predominant.
The most common types of lesions were nodulo-ulcerated
followed by nodular and the most of lesions' sites
were lower limb followed by upper limb. The single
lesions were predominant and the majority of lesion
sizes were 0.5 cm. We concluded that Wadi Hadramout
is an endemic region of cutaneous leishmania.
1. García-Almagro D. Lesihmaniasis
cutánea. Actas Dermosifiliogr. 2005;96:1---24.
2. Desjeux P. Leishmaniasis: Current situation
and new perspectives.
Comp Immunol Microbiol Infect Dis 2004; 27: 305-318.
3. WHO. Leishmaniasis: the global trend[Online].
Available from:
http://www.who.into /neglected_disease/integrated-media_
Leishmaniasis/en/index.html. [Accessed on 2009].
4. Herwaldt BL, Magill AJ. Leishmaniasis, Cutaneous,
Infectious
diseases related to travel, Centers for Disease
Control and
Prevention, Traveler's health. Yellow book, 2012;
Chapter 3.
5. UNDP (2007) Yemen Poverty Assessment Report
United Nations Development
Programme. The government of Yemen, the World
Bank, and the United Nations Development Program.
6. Yemen Tourism Promotion Board. Hadramout governorate.
Available from: http://yementourism.com/services/touristguide/detail.php?ID=2048
7. Kenner JR, Aronson NE, Benson PM. The United
States Military and leishmaniasis. Dermatol Clin.
1999; 17: 77-92.
8. TDR Strategic Direction for research: Leishmaniasis.
2002; Available from: www.who.int/tdr.
9. Manzur A. Cutaneous leishmaniasis. J Pak Assoc
Dermatol. 2005; 15: 161-71.
10. Weigle KA, de Davalos M, Heredia P et al.
Diagnosis of cutaneous and mucocutaneous Leishmaniasis
in Colombia. A comparison of seven methods. Am
J Trop Med Hyg. 1987; 36: 489-96.
11. McGregor A. WHO warns of epidemic of Leishmania.
Lancet. 1998; 351: 575.
12. Bryceson ADM, Hay RJ. Parasitic Worms and
Protozoa. In: Champion RH, Burton JL, Burns DA,
Breathnach SM, eds. Textbook of Dermatology, 6th
edn. Oxford: Blackwell Science; 1998. p. 1377-1422.
13. Giudice P, Marty P, Lacour JP, Perrin C, Pratlong
F, Haas H, Dellamonica P, Le Fichoux Y. Cutaneous
leishmaniasis due to Leishmania infantum. Case
reports and literature review. Arch Dermatol.
1998;134:193-198.
14. Siriwardena HV, Udagedara CU, Karunaweera
ND. Clinical features, risk factors and efficacy
of cryotherapy in cutaneous leishmaniasis in Sir
Lanka. Ceylon Med J.2003;48:10-12.
15. Kheirandish F, Sharafi AC, Kazemi B, Bandehpour
M, Tarahi MJ, Khamesipour A. First molecular identification
of Leishmania species in a new endemic area of
cutaneous leishmaniasis in Lorestan, Iran. Asian
Pacific Journal of Tropical Medicine. 2013; 713-717
16. Kimutai A, Ngure PK, Tonui WK, Gicheru MM,
Nyamwamu LB. Leishmaniasis in Northern and Western
Africa: a review. Afr J Infect Dis. 2009;3:14-25.
17. Aara N, Khandelwal K, Bumb RA, Mehta RD, et
al. Clinico-Epidemiologic Study of Cutaneous Leishmaniasis
in Bikaner, Rajasthan, India. Am J Trop Med Hyg.
2013 Jul 10; 89(1): 111-115.
18. Srivastava D, Vyas MC, Joshi CK. Clinico-epidemiological
study of cutaneous leishmaniasis in Bikaner (Rajasthan).
J Commun Dis. 1987; 19:326-331
19. Sharma NL, Mahajan VK, Kanga A, Sood A, Katoch
VM, Mauricio I, Singh CD, Parwan UC, Sharma VK,
Sharma RC. Localized cutaneous leishmaniasis due
to Leishmania donovani and Leishmania tropica:
preliminary findings of the study of 161 new cases
from a new endemic focus in Himachal Pradesh,
India. Am J Trop Med Hyg. 2005;72:819-824.
20. Ali Raza Syed, Shahbaz Aman, Ijaz Hussain,
Syed Atif Hasnain Kazmi. Kashmor: focus of cutaneous
leishmaniasis. Journal of Pakistan Association
of Dermatologists 2006; 16: 147-150.
21. Mishri Lal Khatri, Nasser Haider, Trentina
Di Muccio, Marina Gramiccia. Cutaneous leishmaniasis
in Yemen: clinicoepidemiologic features and a
preliminary report on species identification.
International Journal of Dermatology. 2006; 45:
40-45
22. Al-Qubati Y. Cutaneous leishmaniasis from
Yemen: treatment with intralesional injection
of sodium stibogluconate with local anesthetic.
Saudi Med J 1997; 18: 433-434
23. Al-Nahhas Samar Anis, Kaldas Rania Magdy.
Characterization of Leishmania Species Isolated
from Cutaneous Human Samples from Central Region
of Syria by RFLP Analysis. Hindawi Publishing
Corporation ISRN Parasitology Volume 2013, Article
ID 308726, 5 pages. Available from: http://dx.doi.org/10.5402/2013/308726
24. Aguado M, Espinosa P, Romero-Maté A,
Tardío JC, Córdoba S, Borbujo J.
Outbreak of Cutaneous Leishmaniasis in Fuenlabrada,
Madrid. Actas Dermosifiliogr. 2013;104(4):334-342
25. Koçarslan S, Turan E, Ekinci T, Yesilova
Y, Apari R. Clinical and histopathological characteristics
of cutaneous Leishmaniasis in Sanliurfa City of
Turkey including Syrian refugees. Indian J Pathol
Microbiol. 211-5
|