|
Renoprotective
evaluations of different angiotensin inhibitors
on Diabetic Nephropathy in Rats
......................................................................................................................................................................
Kawa F. Dizaye (1)
Asmaa A. Ahmed (2)
(1) PhD. Head of Department
of Pharmacology, College of Medicine. Hawler Medical
University, Erbil, Iraq
(2) MSc. Rizgary Teaching Hospital, Ministry of
Health, Erbil, Iraq
Correspondence:
Prof. Dr. Kawa Dizaye
Professor of Pharmacology
Hawler Medical University, Erbil, Iraq
Tel: 009647504452392
Web: hmu.edu.iq
Email:
kawa.dizaye@hmu.edu.iq
|
ABSTRACT
Background: This study was designed
to compare the effectiveness of different
angiotensin inhibitors; direct renin inhibitor
(Aliskiren), angiotensin-converting enzyme
inhibitors (Ramipril) and angiotensin II
receptor blocker (Irbesartan) in prevention
and treatment of nephropathy in a group
of rat diabetic nephropathy in rats.
Methods: Thirty rats were divided into
two groups. The first group consisted of
6 rats which were considered as the normal
control group. The second group included
24 induced diabetic rats. The diabetic model
rats were subdivided into four subgroups
of six rats each. The first subgroup served
as a positive control. The second, third
and fourth subgroup received Ramipril, Irbesartan
and Aliskiren respectively.
Results: Diabetic nephropathic rats
showed a significant increase in blood glucose
level, blood pressure, heart rate, serum
urea, serum creatinine, in addition to deteriorating
renal functions including (urine flow, glomerular
filtration rate, Na+ and K+ excretion rate,
albumin and creatinine in the urine). The
administration of (Ramipril, Irbesartan,
and Aliskiren) caused a significant reduction
in blood pressure, blood glucose, serum
urea, Na+ and K+ excretion rate, with a
significant improvement in urine flow and
glomerular filtration rate. All three drugs
induced a significant elevation in serum
K+ concentration.
Conclusion: Administration of different
angiotensin inhibitors (ramipril, irbesartan,
& aliskiren) could slow the progression
of nephropathy in alloxan induced diabetic
rats. Both ramipril and irbesartan have
the same renoprotective effects for most
parameters.
Key words: Diabetic nephropathy, Aliskiren,
Irbesartan, Ramipril
|
Diabetic nephropathy is a major
microvascular complication of diabetes, representing
the leading cause of end stage renal disease in
the world. Diabetic nephropathy is characterized
by a progressive increase in urinary albumin excretion
(microalbuminuria) and a decline in glomerular
filtration rate (GFR), which occurs in association
with an increase in blood pressure, ultimately
leading to end stage renal disease (1, 2).
Basic and clinical research supports the use of
renin angiotensin aldosterone system (RAAS) inhibitors
in diabetic nephropathy (3, 4, 5).
Several basic and clinical studies, mainly in
diabetic patients, have provided evidence that
some antihypertensive agents that inhibit the
renin angiotensin aldosterone system (RAAS), like
angiotensin II type 1 receptor blockers (ARB)
and angiotensin-converting enzyme inhibitors (ACEI),
are renoprotective (6, 7). The reno-protection
provided by these drugs seems at least partly
independent of BP lowering and related perhaps
to the inhibition of the RAS (8, 9, 10).
Several mechanisms participate in the renal protection
afforded by angiotensin inhibitors. ACEIs increase
the permeability selectivity of the filtering
membrane, thereby diminishing exposure of the
mesangium to proteinaceous factors that may stimulate
mesangial cell proliferation and matrix production,
two processes that contribute to expansion of
the mesangium in diabetic nephropathy. Since angiotensin
II is a growth factor, reductions in the intrarenal
levels of angiotensin II may further attenuate
mesangial cell growth and matrix production (11,
12, 13).
Thus, there do not appear to be significant differences
between ACEI and ARBs in type 2 diabetic patients
with nephropathy based on a small number of comparison
studies.
Other studies in hypertensive type 2 diabetics
with early nephropathy comparing ACEIs and ARBs
have also failed to show significant differences
in the effects of these two drug classes on BP
and urinary albumin excretion (14, 15). Only a
few studies have addressed the question of whether
ACE inhibitors are better than ARBs or vice versa.
This study is designed to compare the effectiveness
of different angiotensin inhibitors, direct renin
(DR) inhibitor (Aliskiren), ACEI (Ramipril) ARBs
(Irbesartan) in prevention and treatment of nephropathy
in rat induced diabetes.
Animals
Healthy adult albino rats of both sexes were used
in the present study. Their weight ranged from
250-300 grams. Rats were grouped and kept in separate
animal cages at the animal house of the College
of Medicine under prevailing atmospheric conditions
(room temperature of about 25c).
The animals were maintained on a balanced diet
(bread, barley, carrots, lettuce, milk) and fresh-water
supply.
Induction of experimental diabetes
Diabetes was induced by a single intraperitoneal
injection of 120mg/kg body weight of alloxan dissolved
in distilled water immediately before injection
16. Alloxan treated animals were allowed to drink
5% of glucose overnight to prevent the potentially
fatal hypoglycemia occurring as a result of massive
insulin release following alloxan injection (17).
Rats showing blood glucose levels above 180 mg/dl
were considered to be diabetic (18) and used for
drug treatment.
Experimental design
Thirty rats were divided into five groups each
consisting of 6 rats in order to study the effect
of different angiotensin inhibitors (Ramipril,
Irbesartan, Aliskiren) during the 21 days study
period:
Group I: Normal control rats given D.W
Group II: Control diabetic rats given D.W
Group III: Diabetic rats given Ramipril
10mg/kg.
Group IV: Diabetic rats given Irbesartan
10mg/kg.
Group V: Diabetic rats given
Aliskiren 10 mg/kg.
The solution of drugs was freshly prepared in
normal saline before administration by an oral
gavage every morning.
Collection of samples
1-Urine
After 3 days, and at the end of drug treatment,
all of the animals were kept in metabolic cages.
Animals were fasted but allowed free access to
water. Urine sample were collected after 24 hours
in urine collecting bottles from which the urine
collected was tested for: Albumin, Creatinine,
Na+ excretion rate and K+ excretion rate, glomerular
filtration rate and others.
2-Blood
At the end of drug treatment, all of the animals
were fasted overnight but allowed free access
to water. The next morning, blood samples were
taken by cardiac puncture into a plastic syringe
under a combination of ketamine in a dose of 75
mg/kg with xylazine in a dose of 10 mg/kg. At
10th day and at the end of experiment (after 21
days), a 24 hours urine collection was carried
out by using the metabolic cage. The urine was
checked for the albumin and total protein by using
Cybow diagnostic kits (DFI co. Ltd, Gimhae- City,
Gyung- Nam, Korea).
Statistical Analysis
All data are expressed as the mean ± standard
error means (M ± SEM). The results were
evaluated by using the Statistical Package for
the Social Sciences (SPSS Version 21) computer
program and the differences in all parameters
between diabetic and non-diabetic rats were analyzed
by a one-way analysis of variables (ANOVA). The
comparison between groups was done using Duncan
test. A change was considered statistically significant
when P<0.05.
The experiments were carried out with the approval
of the ethic committee of Hawler Medical University/college
of Medicine.
Effect
of Ramipril, Irbesartan, and Aliskiren on the
blood pressure and heart rate of diabetic rats
In alloxan-induced diabetic rats, a significant
high elevation in blood pressure was seen when
compared to the normal control group, Table 1.
The heart rate of diabetic rats was moderately
higher than that of the normal control. A significant
reduction in blood pressure was observed following
oral 10 mg/kg administration of all the angiotensin
inhibitors (Ramipril, Irbesartan, and Aliskiren)
when compared to the diabetic group. Table (1).
Ramipril and aliskiren treated group had a significant
reduction in their heart rate, while irbesartan
caused non-significant changes when compared to
the diabetic group.
Table 1: The effects of 10 mg/kg of angiotensin
inhibitors on the blood pressure & heart rate
of the diabetic rats
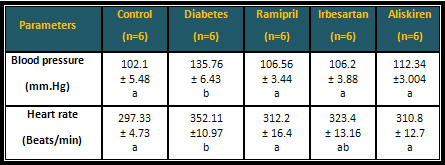
* Similar letters indicate no significant differences.
* Different letters indicate significant differences
at P < 0.05.
Effect of angiotensin inhibitors on the renal
function of diabetic rats
The urine flow of the diabetic rats was significantly
higher than the normal control group. Aliskiren
caused a significant reduction in the urine flow
when compared to the diabetic rats, while ramipril,
and irbesartan produced a non-significant reduction
in the urine flow when compared with both groups.
While the glomerular filtration rate (GFR) of
diabetic rats was found to be significantly lower
than normal rats. Angiotensin inhibitors (Ramipril,
Irbesartan, & Aliskiren) induced a significant
improvement in the GFR when compared to the diabetic
group Table (2).
In alloxan-induced diabetic rats there was a marked
elevation in albuminuria when compared to the
control animals. Daily oral administration of
angiotensin inhibitors for 21 days caused a significant
reduction in albumin excreted through urine when
compared to the diabetic group.
Table 2: The effects
of 10 mg/kg of angiotensin inhibitors on the urine
flow, GFR, and albuminuria of the diabetic rats
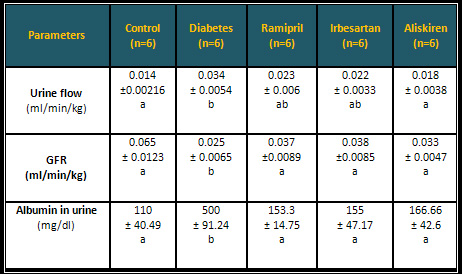
* Similar letters indicate
no significant differences.
* Different letters indicate significant differences
at P < 0.05.
The effect of different angiotensin
inhibitors on Na+ concentration in the urine,
were non-significantly reduced in comparison to
the diabetic animals, although the urinary Na+
concentration did not return to the normal value.
Table (3). The Irbesartan treated rats did not
show a significant improvement in Na+ excretion
rate, while Ramipril and Aliskiren treated rats
induced a significant reduction in Na+ excretion
rate. As shown in Table (3) there was a significant
reduction in Na+ serum concentration level of
angiotensin inhibitors treated rats when compared
to the diabetic rats. In comparison to the diabetic
rats, the percentage of Na+ reabsorption in the
angiotensin inhibitors treatment groups were non-significantly
reduced. Table (3).
Table 3: Effects of angiotensin inhibitors
on the renal excretion of Na+ of the diabetic
rats
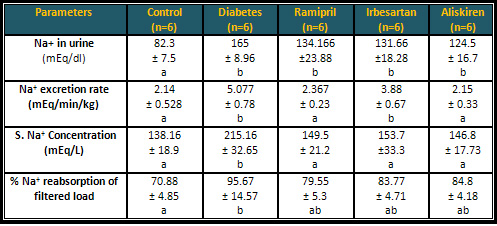
* Similar letters indicate no significant differences.
* Different letters indicate significant differences
at P < 0.05.
Effect of angiotensin inhibitors on the renal
excretion of K+ of the diabetic rats
Following the induction of diabetes by alloxan,
there was a reduction in K+ urine concentration
accompanied by an increase in the urinary potassium
excretion rate. There was a significant elevation
in K+ urine concentration in the groups which
received different angiotensin inhibitors in comparison
with diabetic group.
The angiotensin inhibitor treated rats showed
a significant decrease in the K+ excretion rate
in comparison to the diabetic rats, albeit not
reaching the normal range. The serum concentration
of K+ was increased significantly in diabetic
and treated rats with angiotensin inhibitors when
compared to the control group. Table (4).
Table 4: Effects of
different angiotensin inhibitors on the renal
excretion of K+ of the diabetic rats
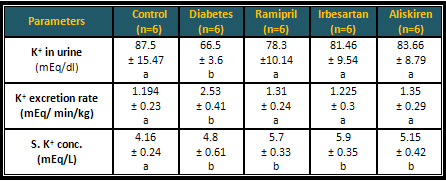
* Similar letters indicate
no significant differences.
* Different letters indicate significant differences
at P < 0.05.
Effect of angiotensin
inhibitors on the biochemical parameters (blood
glucose, serum urea, & serum creatinine) of
the diabetic rats
Following the treatment of diabetic animals with
angiotensin inhibitors Ramipril, Irbesartan, and
Aliskiren at a dose of 10 mg/kg for 21 days, a
significant reduction in the blood glucose and
serum urea were noticed when compared to the diabetic
group. The ramipril, irbesartan, and aliskiren
did not significantly change the serum creatinine
in comparison to the diabetic rats. Table (5).
Table 5: Effect of angiotensin inhibitors on
the biochemical parameters of the diabetic rats
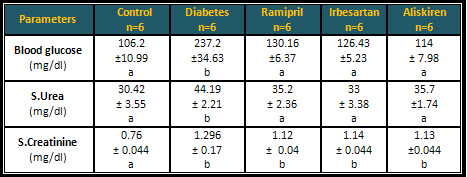
* Different letters indicate significant differences
at P < 0.05.
Several randomized trials have
shown that improved glycemic control in both type
1 and 2 diabetic patients decreases the risk of
diabetic nephropathy and other complications.
Although significant improvement in the treatment
of diabetic nephropathy has occurred over the
past 25 years, as a result, pharmacological inhibition
of the RAS has been proposed as a key strategy
in reducing kidney damage beyond the predicted
effects as a result of blood pressure reduction.
(19, 20, 21).
In diabetic rats, a definite and elevated blood
pressure was seen when compared to the normal
control group, while the heart rate of diabetic
rats was moderately higher than that of the normal
group. The result obtained from experiments on
rats through detecting the effect of (Ramipril,
Irbesartan, and Aliskiren) on blood pressure and
heart rate, showed that there was a statistically
significant decrease in blood pressure with a
non-significant decrease in heart rate. Ramipril
and irbesartan were better than aliskiren in decreasing
Blood pressure. The hypotensive effect of different
angiotensin inhibitors may be explained by the
vasodilating effects of ACEI on the glomerular
efferent arterioles, where it prevents the Ang-II
formation (22). Inhibition of angiotensin lowers
systemic vascular resistance and blood pressure;
this is not surprising when the renal vessels
are exceptionally sensitive to the vasoconstrictor
actions of angiotensin II (23). Angiotensin inhibitor
increases renal blood flow without increasing
GFR; thus reducing the filtration fraction. Both
the afferent and efferent arterioles are dilated
as well as causing systemic arteriolar dilatation.
ACEI increases the compliance of large arteries,
which contributes to systolic pressure reduction
(24).
The urine flow of the diabetic rats was significantly
higher than the normal control group, while the
glomerular filtration rate (GFR) of diabetic rats
was found to be significantly lower than in the
normal rats. In the present study, the result
obtained from the experiment on rats for detecting
the effect of different angiotensin inhibitors
(Ramipril, Irbesartan, and Aliskiren) on urine
flow and glomerular filtration rate, showed a
significant improvement in the urine flow and
GFR. Both ramipril and irbesartan had a superior
renoprotective effect than that of aliskiren.
The renal protection effect of different angiotensin
inhibitors may be explained by ACEI probably attenuating
the progression of renal insufficiency in patients
with a variety of nondiabetic nephropathies, and
may arrest the decline in GFR even in patients
with severe renal disease (25, 26, 27). Normally,
GFR is slightly reduced by angiotensin II; however,
during renal artery hypotension, the effects of
angiotensin II on the efferent arteriole predominate,
leading to increased renal blood flow, hence increasing
GFR. Therefore, blockade of the renin-angiotensin
system may cause acute renal failure in patients
with bilateral renal artery stenosis and in patients
with unilateral stenosis who have only a single
kidney (7). Angiotensin II variably influences
GFR via several mechanisms such as constricting
the afferent arterioles, which reduces intra-glomerular
pressure and GFR, or by contracting the mesangial
cells, which decreases the capillary surface area
within the available glomerulus which subsequently
leads to decrease GFR, and it could be due to
constricting effect on the efferent arterioles,
which increases intra-glomerular pressure which
increases GFR (28, 29).
The result of this experiment is in agreement
with a study by Weidmann et al (1995) who concluded
that GFR is better preserved in ACEI treated groups
(30). Furthermore, Lebovitz et al (1996) (31)
declared that enalapril prevented falling in GFR
in hypertensive patients. However, the result
of the present study does not agree with Kasiske
et al (1993) who found that ACEI is more superior
to B blockers in decreasing GFR among diabetic
patients (32). Parving and Rossing (1994)) concluded
that lisinopril has no significant effects in
decreasing GFR in diabetic nephropathic patients
33 . Moreover, Barnett et al (2005) showed that
the rate of GFR decrease was equivalent in both
enalapril and telmisartan treated patients (34).
In the present study a marked elevation in albuminuria
was seen in diabetic rats. Increased glomerular
pressure associated with diabetes can be enhanced
by aII-mediated constriction of the glomerular
arterioles, causing further elevation in microcirculatory
pressure within the glomerulus, and leading to
excretion of albumin, and thus to the development
of microalbuminuria and proteinuria (35). While
after the oral administration of (ramipril, irbesartan
and aliskiren) a significant reduction in urinary
albumin was noticed. In addition, both ramipril
and irbesartan better reduced the albumin in the
urine. This result is in agreement with studies
conducted by Chan et al (2000), and Jerums et
al (2001) who reported that treatment with ACEI
& aliskiren decrease albumin excretion rate
(36, 37).
Studies in streptozotocin diabetic rats have demonstrated
that both AIIB and ACEi blocked the development
of hypertension and significantly decreased albuminuria
38. Whereas in the DETAIL (Diabetic exposed to
telmisartam and enalapril) study there were no
significant differences in albumin excretion rate
in both enalapril and telmisartan treated patients
(34).
Several mechanisms have been suggested for antiproteinuric
effects of RAS inhibition. First, it may be related
to a reduction in intraglomerular blood pressure
independently of systemic blood pressure by vasodilatation
preferentially of the postglomerular arterioles
(39). Second, RAS inhibition may improve the charge
and size selectivity of the glomerular membrane
(40), which may be related, in part, to reduced
loss of glomerular nephrin, which has been suggested
to play a central role in the function of the
glomerular filtration barrier (41).
The administration of both ramipril and aliskiren
induced a significant change in Na+ excretion
rate, while irbesartan did not show any significant
improvement in diabetic rats. On the other hand
the effect of ramipril, irbesartan, and aliskiren
on the Na+ concentration in the urine was non-significant.
There was a non - significant reduction in the
level of serum Na+ concentration in all treated
rats. The percentage of Na+ reabsorption in the
angiotensin inhibitor treatment group was non
- significantly reduced but still lower than the
control group.
However, it has been suggested that angiotensin
II can act presynaptically to potentiate the release
of norepinephrine from sympathetic nerve terminals
and thus enhancing the renin release from the
renal tubule (42, 43). The rise in sodium level
in diabetic rats could be related to the fact
that angiotensin II stimulates the zona glomerulosa
of the adrenal cortex to increase the synthesis
and secretion of aldosterone which acts on the
distal and collecting tubules to cause retention
of Na+ and excretion of K+ and H+. The stimulant
effect of angiotensin II on aldosterone synthesis
and release is enhanced under conditions of hyponatremia
or hyperkalemia and reduced when concentrations
of Na+ and K+ in plasma are altered in the opposite
directions (44). Very low concentrations of angiotensin
II stimulate Na+/H+ exchange in the proximal tubule;
an effect that increases Na+, Cl-, and angiotensin
II may reduce Na+ excretion in part by diminishing
medullary blood flow.
In the present study, the significant decrease
in the K+ excretion rate accompanied by a non-significant
rise in the serum K+ level were detected following
administration of ramipril, irbesartan, and aliskiren.
These effects could be explained by suppression
of endogenous aldosterone and worsening kidney
function (45). Despite some reduction in the concentration
of aldosterone, significant K+ retention is rarely
encountered in patients with normal renal function
who have not been taking other drugs that cause
K+ retention (46).
In this study, the level of blood glucose in diabetic
rats was significantly increased when compared
to the control group. This result in accordance
with studies of Bilal et al (1998), Azuma et al
(2007) who suggested that elevated blood glucose
levels in diabetes are caused by a defect in production
and or secretion of the hormone insulin (47, 48).
In this study the elevation of blood glucose level
indicate that this effect is caused by the direct
influence of alloxan on pancreatic beta cells.
Treatment with angiotensin inhibitors Ramipril,
Irbesartan, and Aliskiren caused a significant
reduction in the blood glucose level of diabetic
rats. However, aliskiren was better in reducing
blood glucose than the other two drugs.
In this study the hypoglycemic effect of angiotensin
inhibitors may be due to increased rate of glucose
uptake into the cell, and to improve glucose metabolism
(49, 50). Clarification of the mechanism of this
effect is in progress. In patients with essential
hypertension, plasma insulin and blood glucose
levels increase together, indicating reduced insulin
sensitivity. Because of this, even without the
onset of diabetes, a latent rise in blood glucose
level may be seen. Angiotensin receptor blocker
and ACEI can improve glucose metabolism via blocking
the inhibitory effect of angiotensin II on insulin
signal transmission (51, 52). On the other hand,
the vasodilatory action of angiotensin inhibitor
may increase the access of insulin and glucose
to the skeletal muscle tissue, the main site of
insulin- mediated removal of glucose 53. The result
of hypoglycemic effects of ramipril, irbesartan,
and aliskiren in the diabetic rats is in agreement
with other studies done by Jacobsen et al (2003),
Lau et al (2004), Dizaye and Rashid (2009) (54,
55, 56). Subsequent studies indicated that telmisartan
also suppressed the new onset of diabetes (53).
In the present study ramiprl, irbesartan, and
aliskiren did not significantly decrease serum
creatinine, and this effect was compatible with
the finding of Lewis et al (2001) who suggested
that the level of serum creatinine was not significantly
changed by irbesartan in nephropathic patients
(21). Along the same lines, are the data from
other studies which showed that serum creatinine
levels did not significantly change in the ACEI
group (57, 58). However, the result of this study
was in disagreement with the study of Brenner
et al (2001), who found that there was 25% reduction
for doubling the serum creatinine level after
using ACEi (20).
Administration of different
angiotensin inhibitors (ramipril, irbesartan,
and aliskiren) could slow the progression of nephropathy
in alloxan induced diabetic rats. Both ramipril
and irbesartan had the same renoprotective effects
for most parameters.
1. Cooper
WO, Hernandez-Diaz S, Arbogast PG, Dudley JA,
Dyer S, Gideon PS, et al. Major congenital malformations
after first-trimester exposure to ACE inhibitors.
New England Journal of Medicine. 2006;354(23):2443-51.
2. Caramori ML, Mauer M. Diabetes and nephropathy.
Current opinion in nephrology and hypertension.
2003;12(3):273-82.
3- Koike H. New pharmacologic aspects of CS-866,
the newest angiotensin II receptor antagonist.
The American journal of cardiology. 2001;87(8):33-6.
4- Koike H, Sada T, Mizuno M. In vitro and in
vivo pharmacology of olmesartan medoxomil, an
angiotensin II type AT1 receptor antagonist. Journal
of hypertension Supplement: official journal of
the International Society of Hypertension. 2001;19(1):S3-14.
5- Mizuno M, Sada T, Kato M, Koike H. Renoprotective
effects of blockade of angiotensin II AT1 receptors
in an animal model of type 2 diabetes. Hypertension
Research. 2002;25(2):271-8.
6- Remuzzi G, Schieppati A, Ruggenenti P. Nephropathy
in patients with type 2 diabetes. New England
Journal of Medicine. 2002;346(15):1145-51.
7- Jafar TH, Schmid CH, Landa M, Giatras I, Toto
R, Remuzzi G, et al. Angiotensin-converting enzyme
inhibitors and progression of nondiabetic renal
disease: a meta-analysis of patient-level data.
Annals of internal medicine. 2001;135 (2):73-87.
8-Brenner G, Stevens C. Pharmacology. Fourth eddition.
Saunders, Elsevier publisher: 2013. P. 96.
9- Parving H-H, Lehnert H, Bröchner-Mortensen
J, Gomis R, Andersen S, Arner P. The effect of
irbesartan on the development of diabetic nephropathy
in patients with type 2 diabetes. New England
Journal of Medicine. 2001;345 (12):870-8.
10- Valderrabano F, Berthoux FC, Jones EH, Mehls
O. Report on management of renal failure in Europe,
XXV, 1994 end stage renal disease and dialysis
report. Population. 1996;52 (65):62.
11- Salvetti A, Mattei P, Sudano I. Renal protection
and antihypertensive drugs. Drugs. 1999;57(5):665-93.
12- Wingard DL, Barrett-Connor EL, Scheidt-Nave
C, McPhillips JB. Prevalence of cardiovascular
and renal complications in older adults with normal
or impaired glucose tolerance or NIDDM: a population-based
study. Diabetes Care. 1993;16(7):1022-5.
13- Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf
S. Renal insufficiency as a predictor of cardiovascular
outcomes and the impact of ramipril: the HOPE
randomized trial. Annals of internal medicine.
2001;134(8):629-36.
14-Lacourcière Y, Bélanger A, Godin
C, Hallé J-P, Ross S, Wright N, et al.
Long-term comparison of losartan and enalapril
on kidney function in hypertensive type 2 diabetics
with early nephropathy. Kidney international.
2000;58(2):762-9.
15- Mogensen CE, Neldam S, Tikkanen I, Oren S,
Viskoper R, Watts RW, et al. Randomised controlled
trial of dual blockade of renin-angiotensin system
in patients with hypertension, microalbuminuria,
and non-insulin dependent diabetes: the candesartan
and lisinopril microalbuminuria (CALM) study.
Bmj. 2000;321(7274):1440-4.
16- Sultan AH, Dizaye KF, Banna HB. Histological,
Immunocytochemical and Biochemical study of the
effect of Adiantum capillus on alloxan induced
diabetic rats.
17- Kumar GPS, Arulselvan P, Kumar DS, Subramanian
SP. Anti-diabetic activity of fruits of Terminalia
chebula on streptozotocin induced diabetic rats.
Journal of health science. 2006;52(3):283-91.
18-Nair R, Shukla V, Chanda S. Assessment of Polyalthia
longifolia var. pendula for hypoglycemic and antihyperglycemic
activity. J Clin Diagn Res. 2007;1:1-3.
19-Rao RP, Jain A, Srinivasan B. Dual therapy
versus monotherapy of trandolapril and telmisartan
on diabetic nephropathy in experimentally induced
type 2 diabetes mellitus rats. Journal of Renin-Angiotensin-Aldosterone
System. 2011;12(3):169-75.
20- Brenner BM, Cooper ME, de Zeeuw D, Keane WF,
Mitch WE, Parving H-H, et al. Effects of losartan
on renal and cardiovascular outcomes in patients
with type 2 diabetes and nephropathy. New England
Journal of Medicine. 2001;345(12):861-9.
21- Lewis EJ, Hunsicker LG, Clarke WR, Berl T,
Pohl MA, Lewis JB, et al. Renoprotective effect
of the angiotensin-receptor antagonist irbesartan
in patients with nephropathy due to type 2 diabetes.
New England Journal of Medicine. 2001;345(12):851-60.
22- Lansang MC, Price DA, Laffel LM, Osei SY,
Fisher ND, Erani D, et al. Renal vascular responses
to captopril and to candesartan in patients with
type 1 diabetes mellitus. Kidney international.
2001;59(4):1432-8
23- Brunton LL, Chabner B, Knollmann BC. Goodman
& Gilman's the pharmacological basis of therapeutics:
McGraw-Hill Medical New York; 2011. 806
24- Cherney DZ, Scholey JW, Jiang S, Har R, Lai
V, Sochett EB, et al. The effect of direct renin
inhibition alone and in combination with ACE inhibition
on endothelial function, arterial stiffness, and
renal function in type 1 diabetes. Diabetes care.
2012;35(11):2324-30.
25- Maschio G, Alberti D, Janin G, Locatelli F,
Mann JF, Motolese M, et al. Effect of the angiotensin-converting-enzyme
inhibitor benazepril on the progression of chronic
renal insufficiency. New England Journal of Medicine.
1996;334(15):939-45.
26- Kshirsagar AV, Joy MS, Hogan SL, Falk RJ,
Colindres RE. Effect of ACE inhibitors in diabetic
and nondiabetic chronic renal disease: a systematic
overview of randomized placebo-controlled trials.
American journal of kidney diseases. 2000;35(4):695-707.
27- Praga M, Gutiérrez E, González
E, Morales E, Hernández E. Treatment of
IgA nephropathy with ACE inhibitors: a randomized
and controlled trial. Journal of the American
Society of Nephrology. 2003;14(6):1578-83.
28- Pelayo JC, Ziegler MG, Blantz RC. Angiotensin
II in adrenergic-induced alterations in glomerular
hemodynamics. American Journal of Physiology-Renal
Physiology. 1984;247(5):F799-F807.
29- Rang HP, Ritter JM, Flower RJ, Henderson G.
Rang & Dale's Pharmacology: With student consult
online access: Elsevier Health Sciences; 2014.
P=358
30- Weidmann P, Schneider M, Böhlen L. Therapeutic
efficacy of different antihypertensive drugs in
human diabetic nephropathy: an updated meta-analysis.
Nephrology, dialysis, transplantation. 1995;10:39-45.
31- Lebovitz HE, Wiegmann TB, Cnaan A, Shahinfar
S, Sica DA, Broadstone V, et al. Renal protective
effects of enalapril in hypertensive NIDDM: role
of baseline albuminuria. Kidney International
Supplement. 1994(45).
32- Kasiske BL, Kalil RS, Ma JZ, Liao M, Keane
WF. Effect of antihypertensive therapy on the
kidney in patients with diabetes: a meta-regression
analysis. Annals of internal medicine. 1993;118(2):129-38.
33- Parving H-H, Rossing P. The use of antihypertensive
agents in prevention and treatment of diabetic
nephropathy. Current opinion in nephrology and
hypertension. 1994;3(3):292-300.
34- Barnett AH, Bain SC, Bouter P, Karlberg B,
Madsbad S, Jervell J, et al. Angiotensin-receptor
blockade versus converting-enzyme inhibition in
type 2 diabetes and nephropathy. New England Journal
of Medicine. 2004;351(19):1952-61.
35- Kunz R, Friedrich C, Wolbers M, Mann JF. Meta-analysis:
effect of monotherapy and combination therapy
with inhibitors of the renin-angiotensin system
on proteinuria in renal disease. Annals of internal
medicine. 2008;148(1):30-48.
36- Chan JC, Ko GT, Leung DH, Cheung RC, Cheung
MY, So W-Y, et al. Long-term effects of angiotensin-converting
enzyme inhibition and metabolic control in hypertensive
type 2 diabetic patients. Kidney international.
2000;57(2):590-600.
37- Jerums G, Allen TJ, Campbell DJ, Cooper ME,
Gilbert RE, Hammond JJ, et al. Long-term comparison
between perindopril and nifedipine in normotensive
patients with type 1 diabetes and microalbuminuria.
American journal of kidney diseases. 2001;37(5):890-9.
38- Sano T, Kawamura T, Matsumae H, Sasaki H,
Nakayama M, Hara T, et al. Effects of long-term
enalapril treatment on persistent microalbuminuria
in well-controlled hypertensive and normotensive
NIDDM patients. Diabetes Care. 1994;17(5):420-4.
39- Imanishi M, Yoshioka K, Konishi Y, Okumura
M, Okada N, Sato T, et al. Glomerular hypertension
as one cause of albuminuria in type II diabetic
patients. Diabetologia. 1999;42(8):999-1005.
40-Andersen S, Tarnow L, Rossing P, Hansen BV,
Parving H-H. Renoprotective effects of angiotensin
II receptor blockade in type 1 diabetic patients
with diabetic nephropathy. Kidney international.
2000;57(2):601-6.
41- Bonnet F, Cooper ME, Kawachi H, Allen TJ,
Boner G, Cao Z. Irbesartan normalises the deficiency
in glomerular nephrin expression in a model of
diabetes and hypertension. Diabetologia. 2001;44(7):874-7.
42- Suzuki Y, Matsumura Y, Egi Y, Morimoto S.
Effects of Losartan, a nonpeptide angiotensin
II receptor antagonist, on norepinephrine overflow
and antidiuresis induced by stimulation of renal
nerves in anesthetized dogs. Journal of Pharmacology
and Experimental Therapeutics. 1992;263(3):956-63.
43- Takishita S, Muratani H, Sesoko S, Teruya
H, Tozawa M, Fukiyama K, et al. Short-term effects
of angiotensin II blockade on renal blood flow
and sympathetic activity in awake rats. Hypertension.
1994;24(4):445-50.
44- Bautista R, Manning R, Martinez F, del Carmen
Avila-Casado M, Soto V, Medina A, et al. Angiotensin
II-dependent increased expression of Na+-glucose
cotransporter in hypertension. American Journal
of Physiology-Renal Physiology. 2004;286(1):F127-F33.
45- Weir R, McMurray JJ, Puu M, Solomon SD, Olofsson
B, Granger CB, et al. Efficacy and tolerability
of adding an angiotensin receptor blocker in patients
with heart failure already receiving an angiotensin-converting
inhibitor plus aldosterone antagonist, with or
without a beta blocker. Findings from the Candesartan
in Heart failure: Assessment of Reduction in Mortality
and morbidity (CHARM)-Added trial. European journal
of heart failure. 2008;10(2):157-63.
46- Yusuf S, Teo KK, Pogue J. Telmisartan, ramipril,
or both in patients at high risk for vascular
events. N Engl J Med. 2008;2008(358):1547-59.
47- ÜSTÜNDA B, Mehmet Ç, ÖZERCAN
IH, NAZIROGLU M, ILHAN N. Angiotensin Converting
Enzyme Activity in the Serum, Lung, Liver and
Kidney in Streptozotocin-Induced Diabetic Rats
and Diabetic Nephropathy. Turkish Journal of Medical
Sciences. 1998;28(3):231-8.
48- Azuma K, Minami Y, Ippoushi
K, Terao J. Lowering effects of onion intake on
oxidative stress biomarkers in streptozotocin-induced
diabetic rats. Journal of clinical biochemistry
and nutrition. 2007;40(2):131-40.
49- Folli F, Kahn CR, Hansen H, Bouchie JL, Feener
EP. Angiotensin II inhibits insulin signaling
in aortic smooth muscle cells at multiple levels.
A potential role for serine phosphorylation in
insulin/angiotensin II crosstalk. Journal of Clinical
Investigation. 1997;100(9):2158.
50-- Folli F, Saad M, Velloso L, Hansen H, Carandente
O, Feener E, et al. Crosstalk between insulin
and angiotensin II signalling systems. Experimental
and clinical endocrinology & diabetes. 1999;107(02):133-9.
51- Furuhashi M, Ura N, Higashiura K, Murakami
H, Tanaka M, Moniwa N, et al. Blockade of the
renin-angiotensin system increases adiponectin
concentrations in patients with essential hypertension.
Hypertension. 2003;42(1):76-81.
52- Fujimoto M, Masuzaki H, Tanaka T, Yasue S,
Tomita T, Okazawa K, et al. An angiotensin II
AT 1 receptor antagonist, telmisartan augments
glucose uptake and GLUT4 protein expression in
3T3-L1 adipocytes. FEBS letters. 2004;576(3):492-7.
53- Ridker PM, Gaboury CL, Conlin PR, Seely EW,
Williams GH, Vaughan DE. Stimulation of plasminogen
activator inhibitor in vivo by infusion of angiotensin
II. Evidence of a potential interaction between
the renin-angiotensin system and fibrinolytic
function. Circulation. 1993;87(6):1969-73.
54- Jacobsen P, Andersen S, Jensen BR, Parving
H-H. Additive effect of ACE inhibition and angiotensin
II receptor blockade in type I diabetic patients
with diabetic nephropathy. Journal of the American
Society of Nephrology. 2003;14(4):992-9.
55- Lau T, Carlsson P-O, Leung P. Evidence for
a local angiotensin-generating system and dose-dependent
inhibition of glucose-stimulated insulin release
by angiotensin II in isolated pancreatic islets.
Diabetologia. 2004;47(2):240-8.
56- Dizaye K, Rashid BZ. Effects of Ramipril on
glycosylated hemoglobin and liver function tests
in hypertensive patients. MIDDLE EAST JOURNAL
OF INTERNAL MEDICINE. 2009.
57- Ravid M, Savin H, Jutrin I, Bental T, Katz
B, Lishner M. Long-term stabilizing effect of
angiotensin-converting enzyme inhibition on plasma
creatinine and on proteinuria in normotensive
type II diabetic patients. Annals of Internal
Medicine. 1993;118(8):577-81.
58- Mann JF, Gerstein HC, Yi Q-L, Franke J, Lonn
EM, Hoogwerf BJ, et al. Progression of renal insufficiency
in type 2 diabetes with and without microalbuminuria:
results of the Heart Outcomes and Prevention Evaluation
(HOPE) randomized study. American Journal of Kidney
Diseases. 2003;42(5):936-42.
|