|
Assisted Vaginal
Deliveries in Far South of Jordan
......................................................................................................................................................................
Mitri Rashed (1)
Areej Bisharat (2)
Bassam Nusair (3)
Majida Al-Sukkar (4)
Najwa Al-Sunna (5)
(1) Mitri Rashed MD JBOG Senior specialist in
Obstetrics & Gynaecology Prince Hashem Bin
Abd-Allah The Second Military Hospital-Aqaba Jordan.
(2) Areej Bisharat MD JBPN Specialist in Paediatrics
& Neonatologist Queen Rania Al-Abdulla children
Hospital-Amman Jordan.
(3) Bassam Nusair MD JBOG Senior Specialist in
Obstetrics & Gynaecology King Hussein medical
centre-Amman Jordan.
(4) Majida Al-Sukkar MD JBOG Specialist in Obstetrics
& Gynaecology King Hussein medical centre-Amman
Jordan.
(5) Najwa Al-Sunna`MD JBPN Senior Specialist in
Paediatrics & Neonatologist, Queen Ranks Al-Abdulla
children Hospital-Amman Jordan.
Correspondence:
Mitri Rashed MD JBOG
Senior specialist in Obstetrics & Gynaecology
Prince Hashem Bin Abd-Allah The Second Military
Hospital-Aqaba
Jordan
Email:
mitrirashed@yahoo.co.uk
|
ABSTRACT
Objective: To determine the rate, indications
and complications of instrumental deliveries
at Prince Hashim Ben Abdullah The Second
Hospital (former name Princess Haya Bent
Al-Hussein), Aqaba, Jordan.
Methods: This retrospective
observational study has been carried out
over a four-year period between 1st January
2012 and 31st December 2015. The medical
records of all patients who underwent instrumental
deliveries were reviewed and analyzed.
Results: During
this four-year period 238 successful instrumental
deliveries were performed out of 9,767 deliveries
with a rate of 2.56%. The commonest instrument
used was vacuum (202/240) and 36 patients
were delivered by forceps. The indications
were; presumed fetal distress (132), prolonged
2nd stage of labor (85) and maternal exhaustion
(21). Maternal complications reported were
postpartum hemorrhage (18) and different
degrees of genital tract tears (28). Fetal
complications registered consisted of 34
cases of which (11) were cases of Erbs palsy,
(12) were cases admitted to NICU for observation
and one case was diagnosed with cerebral
palsy.
Conclusion: Our
study showed a lower rate of operative vaginal
delivery in comparison to the international
figures. This may be attributed to the lack
of epidural anesthesia which increases the
incidence of instrumental deliveries, in
addition to the simple experience of the
attending residents who fear possible complications
of applying these instruments and the potential
subsequent litigation. The complications
reported in our study were expected in assisted
vaginal deliveries (AVD) and mimic those
mentioned in the literature.
Key words: instrumental
deliveries, indications, complications, Jordan |
Assisted vaginal delivery offers
the option of an operative procedure to safely
and quickly remove the infant, and to safeguard
mother and obstetrician from a difficult or even
hazardous situation when spontaneous vaginal delivery
does not occur within a reasonable time. A successful
assisted or operative vaginal delivery trial avoids
caesarian section with its attendant uterine scar
and implications for future pregnancies. It also
avoids potential birth asphyxia from prolonged
fetal and cord compression. Reviews of delivery
statistics showed considerable variation in the
incidence of assisted vaginal deliveries, but
the range is usually between 10% and 20% of all
deliveries (1, 2). Whether the method employed
is the ventouse (vacuum extractor) or the obstetrics
forceps, the operator can expect optimal results
only when careful attention is given to the
indications, prerequisites and performance of
the procedure.
This retrospective observational
study included all pregnant ladies booked in the
antenatal clinic and unbooked patients admitted
in early labor for whom assisted vaginal delivery
was indicated later. It also included all those
cases coming in to the emergency room at any time
for whom assisted vaginal delivery was indicated.
The medical records of all patients and their
babies who underwent AVD at Prince Hashem Ben
Abdullah The Second hospital between 1st of January
2012 and 31st of December 2015 were reviewed and
analyzed.
The age, parity and the indication for the AVD
were recorded. The decision to undertake an AVD
was in every case made by the obstetrician in
charge. The procedure was
performed by the specialist or by attending resident.
All AVDs were performed using either metallic
cup (Malstrom or Birds) or obstetrician forceps
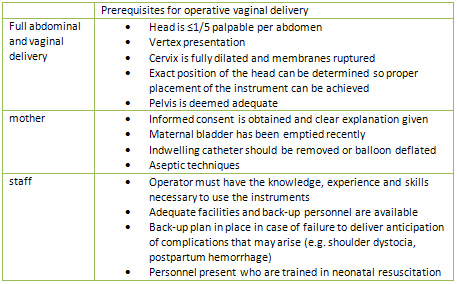
(long and short Simpson or Wrigly's). The prerequisites
of application are mentioned in (Table 1) (2).
Either Foley catheter or prostin vaginal tablets
(dinoprostone 3mg) or both were used for induction
of labor in indicated cases. Artificial rupture
of membranes or oxytocin or both were used for
augmentation of labor. Pethidine was the main
analgesic given in the 1st stage of labor, and
local analgesics (lidocaine) infiltrated in the
perineum were the pain killers of the second stage.
Table 1
If there were insufficient uterine
contractions in the 2nd stage of labor, this was
corrected using oxytocin infusion to achieve regular
uterine contractions; (three or more uterine contractions
in 10 minutes each lasting >40 seconds). AVD
was done when the 2nd stage of labor was prolonged
for more than 2 hours for nullipara patients and
more than one hour for multipara patients. Presumed
fetal distress was diagnosed by electronic fetal
monitoring which has a higher false positive rate
for detection of fetal hypoxia and acidosis. Further
investigation by fetal blood scalp sampling and
PH measurement is usually indicated to avoid unnecessary
intervention, but unfortunately our unit does
not have a fetal blood PH sampling machine. Maternal
exhaustion and fatigue was diagnosed when the
mother's pushes were insufficient to descend the
presenting part further.
Unsuccessful trial of AVD was elicited with failure
of descent of the presenting part after three
successive pulls or five pop-offs of the vacuum
cup with resort to lower uterine segment caesarian
section.
Maternal complications that were reported from
the medical records of the patients constituted
different degrees of vaginal or
perineal tears and postpartum hemorrhage. The
diagnosis of the postpartum hemorrhage relied
on estimation of blood loss >500cc with drop
of PCV value >5. Fetal complications
were reported by reviewing the medical records
of the babies.
The aim of this study was to determine the rate,
indications and short term maternal and neonatal
complications of AVD in two military hospitals
in the south of Jordan.
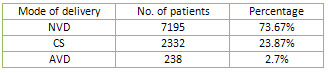
In this study, a total of 8,791
deliveries in the years 2012 to 2015 were performed
after excluding preterm deliveries and breech
deliveries (976 case). During the study period
238 successful instrumental deliveries were done
with a rate of 2.7%. The mean maternal age of
the study population was 26.45 years and the mean
parity was 1.1 (Table 2). Out of these 238 patients,
136(57.14%) were primigravidas; the remaining
were multigravida (parity range 1-8).
Table 2
The main instrument used was metallic vacuum cup
(202/238) and (36/238) deliveries were performed
using obstetrics forceps. 20 LUSC/S were undergone
after unsuccessful trials of vacuum assisted vaginal
deliveries. A zero failure rate was found using
the forceps. The commonest indication for AVD
was presumed fetal distress (Table 3).The maternal
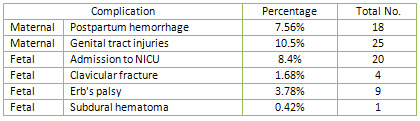
and fetal complications reported are shown in
(Table 4) where the commonest maternal complication
was different degrees of genital tract tears (25/238)
and three of these patients needed repair under
general anesthesia. The postpartum hemorrhage
which afflicted 18 patients was mainly secondary
to genital tract trauma followed by the uterine
atony and the majority of these ladies received
blood products.
Fetal complications registered consisted of (11)
cases of Erbs palsy, (12) cases were admitted
to NICU for observation and one case of cerebral
palsy (Table 5).The main cause of new born admissions
to the neonatal intensive care unit (NICU) was
for observation to rule out sepsis due to prolonged
premature rupture of membranes. All the admissions
were discharged home well except three cases.
One was referred to King Hussein Medical Center
due to suspected intestinal obstruction, another
was diagnosed to have Rh incompatibility, and
the third one was diagnosed to have cerebral palsy
on follow up visits.
Table 3
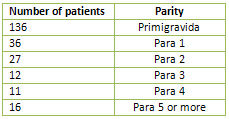
Table 4
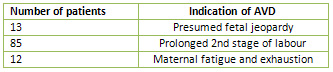
Table 5
Overall instrumental delivery
rates worldwide are around 10%, but vary widely
from 1.5 of deliveries in Czech Republic to 15%
in Canada. Even within a single country, the range
is wide (e.g. in Scotland, from 4% to 26% in primiparous
women(3), and in the United States 1-23 percent(4).
The precise incidence of operative vaginal delivery
in the United States is unknown, but forceps or
vacuum delivery was coded over the birth certificate
as the method of delivery for 8% of vaginal births
in 2002(5). The total rate of operative vaginal
delivery in 2014, the last year for which complete
data are available in the United States, was only
3.1%. Obstetric forceps were used in 0.57% of
deliveries and 2.64% were delivered via the vacuum
extractor (6). So in most countries the overall
rate is reasonably constant, but there is a gradual
move away from forceps towards vacuum due to the
perception that vacuum is easier and safer to
use.
In our study the incidence of instrumental deliveries
was 2.7% which is much below the average rate;
this might be attributed to more than one factor.
First, the lack of use of regional anesthesia
as routine in the labour rooms. This is now well
documented to increase the incidence of instrumental
deliveries (7,8) by several mechanisms, one mechanism
being the reduction in serum oxytocin level which
results in a weakening of uterine activity and
this may be due in part to intravenous fluid infusion
being given before epidural analgesia. Maternal
effort at expulsion can also be impaired, causing
fetal malposition during descent (9). Five trials
that included 2703 nulliparous women were analyzed
by Sharma and colleagues (2004). Women given epidural
analgesia had a two fold increase in rate of instrumental
delivery compared with those given parenteral
analgesia - 13 versus 7 % ( 8).
The second factor participating in the low rate
in our set up is the lack of experience of the
delivery room attending obstetricians (most of
the time they are residents).
Lastly, the fear of potential neonatal complications
and possible litigation in courts makes them resort
to the abdominal delivery as a reasonable alternative.
Maternal indications of operative vaginal delivery
are most commonly due to maternal distress, maternal
exhaustion, or undue prolongation of the second
stage of labor (2, 12). Fetal indications commonly
encountered are malposition of the fetal head,
with relative dystocia which occurs more frequently
with regional anesthesia (4). Fetal distress is
a commonly cited indication. This expression is
subject to varied interpretation which may range
from a brief bradycardia to prolonged late decelerations
with acidosis. So a "presumed fetal jeopardy"
may be a preferable term(1), in conjunction with
recording of as precise a description of the situation
as possible in order to validate the indication.
Presumed fetal jeopardy was the main indication
of operative vaginal delivery in our study (132/238)
55.46% followed by prolonged second stage of labor
(85/238) 35.7%
Most of the complications of AVD have also been
reported following spontaneous vaginal and even
abdominal deliveries, but their incidence is greater
with AVD(1).
Maternal complications are usually those of soft
tissue trauma and tend to be reported more frequently
with the use of forceps than with ventouse (12);
they can include uterine, cervical or vaginal
injury, laceration or hematomas and the consequent
risk of postpartum hemorrhage. In this study 25
patients had genital tract injuries (perineal,
vaginal, and cervical) and 18 cases had postpartum
hemorrhage (7.56%), of which 11 were secondary
to genital tract trauma, and the remainder were
caused by uterine atony.
Data from several sources, including several large
randomized trials performed in industrialized
countries, indicate that the prevalence rate of
PPH of more than 500 mL is approximately 5% when
active management is used (which is adopted in
our hospitals) versus 13% when expectant management
is used(13). Cervical laceration is most commonly
associated with forceps delivery, and the cervix
should be inspected following all such deliveries.
Vaginal sidewall laceration is also most commonly
associated with operative vaginal delivery.
Fetal complications of forceps delivery include
transient facial marks, facial nerve palsies and
fracture of facial bone or skull (1). Injuries
from vacuum include minor and occasionally severe
scalp injuries, including scalp bruising, abrasions,
lacerations, cephalhematoma, subgaleal hematoma
and intracranial hemorrhage (12). 9 babies whose
deliveries were complicated by shoulder dystocia
suffered from Erbs palsy with concomitant clavicular
fractures in 4 of them. Shoulder dystocia and
its peripheral nerve palsy complications (Erb's
palsy) are slightly more common after AVD than
after spontaneous delivery. The risk of shoulder
dystocia is now mainly with vacuum use. This may
be related to the physics of extraction, specifically
the vector of force generated by the vacuum cup
versus forceps(10,12,13). Unfortunately we could
not elicit the incidence of shoulder dystocia
in this study due to the poor notes in the medical
records.
The only severe fetal complication reported was
for a baby who was an outcome of vacuum delivery
with an indication of fetal distress and cord
prolapse. This baby was delivered with a low Apgar
score at 5 minutes and had bilateral cephalhematoma
and was ventilated for three days. His brain CT
scan showed subdural hematoma and he was diagnosed
to have hypotonic ataxic cerebral palsy on follow
up visits. In literature the reported incidence
of fetal death or severe fetal injury from vacuum
extraction is low, ranging from 0.1-3 cases per
1,000 procedures (10).
Our study showed a lower rate
of operative vaginal delivery in comparison to
the international figures. This may be attributed
to the lack of epidural anesthesia which increases
the incidence of instrumental deliveries, in addition
to the simple experience of the attending residents
who fear possible complications of applying these
instruments and the consequent litigation. The
complications reported in our study were expected
in assisted vaginal deliveries and mimic those
mentioned in the literature.
1. David K. James, Philip J. STEER; Carl P. Weiner;
Bernard Gonik. High Risk Pregnancy, Management Options.
In: Robert Hayashi, Assisted Vaginal Delivery. 4th
edition. Saunders, an imprint of Elsevier 2011
2. Royal College of Obstetricians
and Gynecologists. Operative Vaginal Delivery.
Guideline No.26 January 2011.
3. John Studd. Progress in Obstetrics
and Gynecology. In: Asma Khalil Pat O'Brien, editor.
Operative Vaginal Delivery. Volume 16. Elsevier
Churchill Livingstone 2005
4. Clark SL, Belfort MA, Hankins
GD, et al. Variation in the rates of operative
delivery in the United States. Am J Obstet Gynecol
2007; 196:526.e1.
5. F. Gary Cunningham; Kenneth
J. Leveno; Steven L. Bloom; John C. Hauth ; Larry
Gilstrap III; Katharin D. Wenstrom, Williams Obstetrics.
In: Forceps Delivery and Vacuum Extraction. 24th
edition. The McGraw-Hill Companies 2014
6. Hamilton BE, Martin JA, Osterman
MJ, et al. Births: Final Data for 2014. Natl Vital
Stat Rep 2015; 64:1.
7. Janye Althaus, Joseph Wax.
Analgesia and Anesthesia in Labor. Obstet Gynecol
Clinic N Am 32(2005)231-244
8.Anim-Somuah M, Smyth R, Howell
C. Epidural versus non-epidural or no analgesia
in labour. Cochrane Database system. Rev 2005;(4):CD
000331.
9. EHC Liu, ATH Sia. Rates of
Caesarian section and instrumental vaginal delivery
in nulliparous women after low concentration epidural
infusions or opioid analgesia: systemic review.
BMJ doi:10.1136/bmj.38097.590810.7C (published
28 May 2004)
10. John P O'Grady; Carolyn Taugher.
Vacuum Extraction. Available from: http:// emedicine.medscape.com/article/271175
11. John R Smith; Barbara G Brennan.
Postpartum Hemorrhage. Available from: http://www.emedicine.com/medtopic3568
12. Royal College of Obstetricians
and Gynecologists. Shoulder Dystocia. Guideline
No.42 December 2005
13. Vincenzo Berghella.
Obstetrics Evidence Based Guidelines. In: Vincenzo
Berghella. Editor. Shoulder Dystocia. First EDITION.
Informa Health 2007
|