|
Association between
maternal anaemia and premature birth
......................................................................................................................................................................
Rema Khlaif
Omosh
Nansi Dari Alfayez
Iman Fayez
Khloud Alajarmeh
Prince Hashim Hospital
Prince Ali Hospital
Jordan
Correspondence:
Rema Khlaif Omosh
Email: remaomosh@yahoo.com
|
ABSTRACT
Objective: This study was designed
to assess the relation between maternal
anaemia in the third trimester and premature
birth.
Methods: A case-control study was
conducted in Prince Hashim hospital and
Prince Ali Hospital in the period between
August 2015 and July 2016. A total of 200
women were included in the study and divided
into two groups. Group A consisted of patients
delivered between 24-37 weeks of gestation
(case group), while Group B consisted of
patients delivered after 37 weeks (control
group). Maternal anaemia was defined as
haemoglobin level < 11g/dL and preterm
delivery was defined as delivery prior to
37 weeks of gestation. Patients with haemoglobinopathies,
systemic diseases, Antepartum haemorrhage
and multiple gestations were excluded from
the analysis.
Results: In Group A, 47 patients
were found to be anaemic while 53 patients
had normal haemoglobin. In Group B, 29 patients
were found to be anaemic while 71 patients
had normal haemoglobin.
Conclusion: It was observed that
maternal anaemia in the third trimester,
at labour, was associated with an increased
risk of prematurity.
Key words: Anaemia, Preterm delivery,
Prematurity
|
Anaemia is one of the most common
nutritional disorders in the world. According
to the WHO criteria, anaemia is defined as a blood
haemoglobin concentration lower than 12 g/dL for
non-pregnant women and lower than 11 g/dL for
pregnant women.(1)
Prevalence of anaemia in Jordan is 20%, but among
pregnant women this percentage reaches 32% according
to a study conducted by the Jordanian Ministry
of Health and UNICEF in 2009.(2)(3)
Iron deficiency anaemia comprises the majority
of all anaemia seen in pregnancy. Other causes
of anaemia include vitamin B12 and folic acid
deficiencies, hereditary anaemia, chronic infections
and inflammations.(4)(5)
Finding an association between anaemia in pregnancy
and pregnancy outcomes has been investigated in
many studies. Jain Preeti et al and Levey et al
observed that mothers with anaemia have higher
rates of preterm deliveries and low birth weight.(6)(7)
The main purpose of the study is to find an association
between anaemia and preterm delivery so that pregnant
patients at risk are identified and effective
management can be taken to prevent and treat anaemia.
Our study was conducted on pregnant
women admitted to the labour ward of Prince Hashim
Hospital and Prince Ali Hospital between August
2015 and July 2016. The initial sample consisted
of 253 patients, from whom we selected all who
met the inclusion criteria, i.e. who were followed
in outpatient department since early pregnancy,
aged between 18-40 years and had a singleton pregnancy.
Patients with multiple gestation, chronic illness,
antepartum haemorrhage and unbooked patients were
excluded and 200 patients remained for analysis.
Data were collected from the interviews conducted
with the patients and medical records; data were
recorded on special forms designed for this purpose.
Information was analysed by using SPSS software.
Blood samples were drawn from patients at admission
and haemoglobin level was estimated using a Sysmex
KX-21 N machine (Swe Lab).
Anaemia in pregnant patients was defined according
to WHO as haemoglobin level below 11g/dL.
Gestational age was calculated using Naegele's
rule as the duration of pregnancy in weeks, i.e.
from the first day of the last menstrual cycle
to the date of delivery, and compared with ultrasound
measurements in the first trimester and at admission.
Preterm birth was defined based on the WHO definition
as delivery prior to 37 weeks of gestation.
The population
of the current study consisted of 200 patients
divided into two groups. Group A comprised of
preterm (cases) whilst Group B consisted of term
(controls). In distribution of patients on the
basis of anaemia, it was found that 47 patients
(47 %) in group A were anaemic and 53 patients
(53%) had normal haemoglobin. In group B, 29 patients
(29%) were anaemic while 71 patients (71%) had
normal haemoglobin. As Table 1 shows, the mean
of haemoglobin in Group A was 10.30 and that of
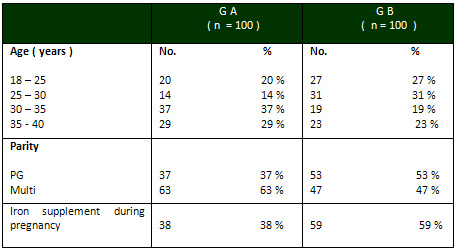
Group B was 11.19 . In distribution of patients
on the basis of parity, in Group A there were
37 (37%) patients who were primigravidas and 63
(63%) patients who were multigravidas, while in
Group B, 53 (53%) patients were primigravidas
and 47 (47%) were multigravidas, as shown in Table
2.
In distribution of patients according to age,
in Group A there were 20 patients (20 %) whose
ages ranged from 18 to 25 years, 14 patients (14%)
in the range of 25-30 years, 37 patients (37 %)
in the range of 30-35 years and 29 patients (29%)
who were aged between 35 and 40 years . In Group
B there were 27 patients whose ages ranged from
18 to 25 years (27 %), 31 patients (31%) aged
25 to 30 years, 19 patients (19 %) in the range
of 30-35 years, and 23 patients (23%) in the range
of 35-40 years, as shown in Table 2.
In distribution of patients according to iron
supplementation during pregnancy, in Group A there
were 38 patients ( 38%) who received iron supplements
and 62 patients (62%) who did not receive iron
supplements. In Group B, there were 59 patients
(59%) who received iron supplements and 41 patients
( 41%) who did not receive iron supplements, as
shown in Table 2.
Table 1: Distribution of patients according to
Hb level
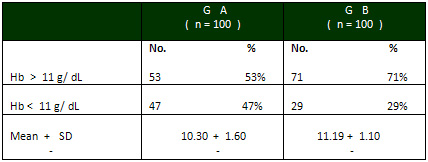
Table 2:. Distribution of patients on the basis
of age, parity and iron supplement
Anaemia is defined as a decrease
in the total circulating red cell mass below the
normal ranges (8).
During pregnancy, iron deficiency and iron deficiency
anaemia are the most common nutritional disorders.
Iron deficiency anaemia comprises 90% of all anaemia
seen in pregnancy(WHO92). Malaria, hookworm infection,
schistomiasis, chronic inflammations and inherited
anaemia are other causes.(1)
Maternal anaemia is associated with premature
delivery, low birth weight (9-11), IUGR (intrauterine
growth retardation), IUD (intrauterine death),
low APGAR score and perinatal death .(12).
In our study, the mean of haemoglobin in preterm
group was 10.30 g/dL, which is lower than that
in the term group, 11.19 g/dL. It was observed
that maternal anaemia evaluated during the third
trimester, i.e. at labour, is a risk factor behind
prematurity. The effect associated with anaemia
remained recognisable even after adjustment for
potential confounding factors.
It was also observed that multiparity and older
age were associated with an increased risk of
preterm delivery.(13)
Our study showed that the percentage of patients
who received iron supplements during pregnancy
was low in the preterm group (38%), while the
percentage in the term group was much higher (59%).
The results of our study were comparable to many
previous studies that investigated the mutual
relation between maternal anaemia and prematurity.
This is exemplified in the study conducted by
Scholl and Hedgier (14) that shows that maternal
anaemia is associated with a 2-3 fold increased
risk of premature delivery.
Based on the results of the current
study, it can be concluded that anaemia is the
most common nutritional deficiency in pregnancy
and it is strongly associated with preterm delivery.
Educational efforts addressing the appropriate
use of prenatal and antenatal care should be initiated
to educate women about their health and the associated
risks during pregnancy, especially anaemia.
1. World Health Organization.
The prevalence of anaemia in women: a tabulation
of available information. 2nd ed. Geneva: World
Health Organization, 1992.
2. Department of Statistics [Jordan] and ICF Macro.
2010. Jordan Population and Family Health Survey
2009. Calverton, Maryland, USA: Department of Statistics
and ICF Macro
3. WHO , UNICIF , UNU . Iron deficiency anaemia
: assessment , prevention and control , a guide
for programme managers , 2001 .
4. Massawe SN (1999) The complexity of anemia in
pregnancy in Dar-es-Salam. Gynaecol Obstet Invest.
47:76-82.
5. Rasmussen KM (2001) Is there a casual relationship
between iron deficiency anemia and weight at birth.
J Nutr. 131:590-630.
6. Jain Preeti, Kural M . Maternal and fetal outcome
in cases of severe anaemia with pregnancy. Int J
Med Appl Sci. 2013;2(3):318-33.
7. Levy a, Fraser D. Maternal anaemia during pregnancy
is an independent risk factor for low birth weight
and preterm delivery. 2005;122(2):182-6.
8. Letshy EA (1995) Blood volume, haematinics, anemia.
Medical disorders in obstetrics practice. Oxford:
Blackwell Science. 33-70.
9. Kumar A, Chaudhary K . Maternal Indicators and
obstetric outcome in the Indian population. J Postgrad
Med. 2010;56:192-5.
10. Malhotra M, Sharma JB. Maternal and perinatal
outcome in varying degrees of anemia. Int J Gynaecol
Obstet. 2002;79:93-100.
11. Steer PJ. Maternal haemoglobin concentration
and birth weight. 2000;71(5):1285-7.
12. Lone FW, Qureshi RN . Maternal anaemia and its
impact on perinatal outcome. 2004;9(4):486-90.
13. R Sehgal , A Kriplani , P Vanamail , L Maiti
, S Kandpal , N Kumar : Assessment and comparison
of pregnancy outcome among anaemic and non anaemic
mothers. 2016.
14. Scholl To, Hediger ML , Fisher RL , Sheare JW
. Anaemia Vs Iron deficiency : Increased risk of
preterm delivery in a prospective study. 1992
|